JAMA Oncol:传统治疗方式的“逆袭” :TACE+放疗治疗晚期HCC患者
2018-04-04 慧语 肿瘤资讯
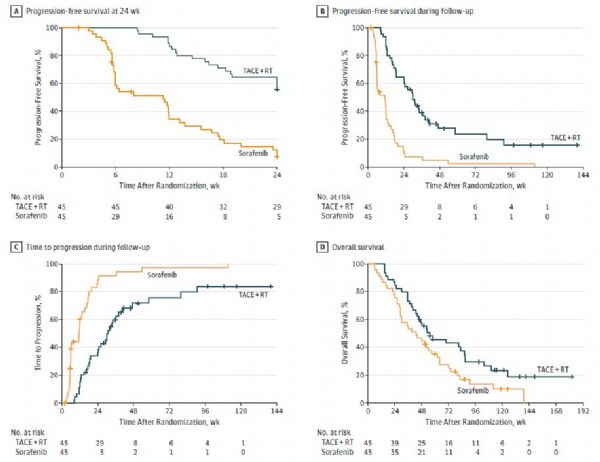
索拉非尼是目前晚期肝细胞癌(HCC)患者的一线治疗药物。近来有研究报道了其它传统的治疗方式,如肝动脉化疗栓塞(TACE)与放疗(RT)联合运用治疗HCC患者,也具备了一定的有效性和安全性。那么传统方式能否“逆袭”成功,请跟随小编一探究竟。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#TAC#
32
#治疗方式#
32
#Oncol#
32
#晚期HCC#
29
#ACE#
0
学习了
82
体部立体定向放射治疗一直在用!
74
#HCC#
29
学习了.谢谢分享
72
谢谢分享学习
76