J CLIN ONCOL :溶瘤病毒对抗脑瘤!临床1期显示:显著延长患者生存期
2018-02-27 Flora 生物探索
“一种常见的感冒病毒经过‘改造’后,能够攻击致命的脑瘤,延长患者的生存期”——这是一项发表在《Journal of Clinical Oncology》期刊上的最新成果。来自于德克萨斯大学MD安德森癌症中心的研究人员刚刚完成了临床Ⅰ期试验,并获得喜人的成绩。
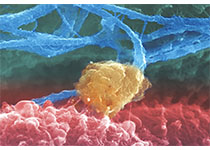
带来这一惊喜的溶瘤腺病毒(oncolytic adenovirus)被命名为“DNX-2401”(Delta-24-RGD),不仅仅可以特异性靶向肿瘤细胞,还具备较强的复制能力,能够进一步刺激宿主的抗肿瘤免疫反应。
来自于MD安德森癌症中心的科学家们针对DNX-2401启动了临床Ⅰ期试验,结果显示,该病毒能够显着延长胶质母细胞瘤复发患者的生存期,其中20%的患者生存期达到3年。通常,胶质母细胞瘤复发的患者只有6个月的中位生存期。这无疑是个好消息。
172%的患者生存期延长
他们共招募37名复发性恶性胶质瘤患者,并分成两组:A组(25人)接受病毒注射,用于评估安全性和有效性;B组(12人)患者在接受病毒注射14天后,将被采集肿瘤样本,用于分析腺病毒的作用机制。
结果显示,A组中有18例患者(72%)的肿瘤减小,总体生存期达到9.5个月。同时,有3名患者的肿瘤得到了95%的减少,且无进展生存期超过3年(其中2名患者的无进展生存期分别达到42.5个月、36.4个月)。
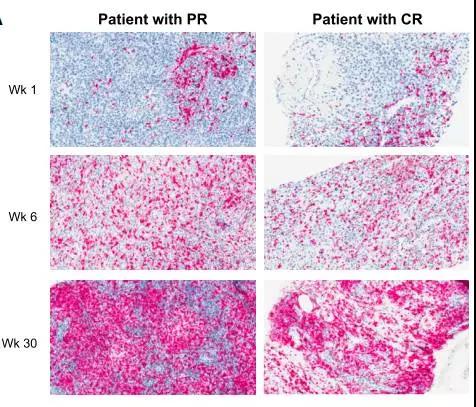
B组结果表明,DNX-2401被证实能够特异性攻击癌细胞,并在肿瘤组织内复制、扩散。而且,这一疗法毒性较小,只有两名患者出现了与治疗相关的轻度副作用。
2腺病毒刺激免疫反应
临床试验表明,腺病毒感染可以激活免疫系统攻击肿瘤。
通常,胶质母细胞瘤不会引起免疫系统的注意,几乎没有T细胞能够穿透肿瘤。现在,溶瘤腺病毒可以通过杀死肿瘤细胞,瓦解肿瘤对于免疫系统的逃逸机制,从而为后者提供多个抗原靶点,最终完全摧毁肿瘤。
研究团队正在优化这一方案,为病毒添加新的因素,从而进一步刺激免疫系统。他们还试图将“智能病毒炸弹”与其他治疗方法结合,例如“DNX-2401+Keytruda”(一款热门的免疫检查点抑制剂),以此评估这一联合增强免疫反应的效果。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#临床1期#
41
#Oncol#
25
#患者生存#
42
#脑瘤#
43
#生存期#
25
学习了.谢谢作者分享!
73