Hepatology:肝内门静脉系统分流术后肝硬度增加与炎症相关,并可预测死亡率
2018-04-24 MedSci MedSci原创
研究表明,系统炎症出现后,TIPS术后,患者肝脏硬度增加的风险增高;是器官衰竭和死亡的预测因素。
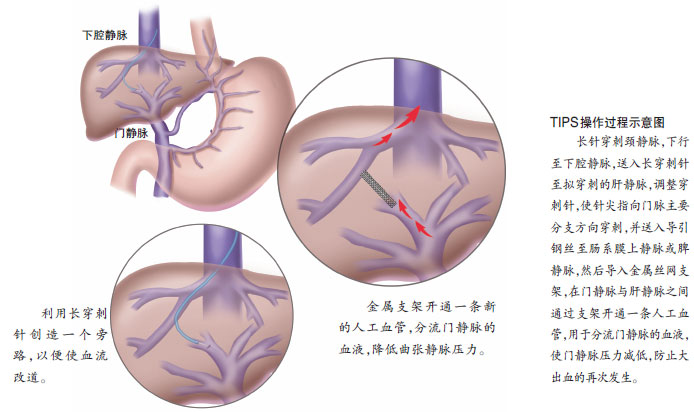
研究背景:经颈静脉内门静脉分流术(TIPS)可以有效治疗门静脉高压症并发症。肝脾僵硬可能能够预测门静脉高压症的出现与否。这项前瞻性研究调查了接受TIPS的患者的肝脏僵硬程度,无论患者是否存在门静脉高压的指征。
研究方法:在83例患者中,16例患者(急性组)在TIPS术前和TIPS后30分钟内进行了瞬时弹性成像检测;67例患者(慢性组)在TIPS术前1天和TIPS术后7天进行了肝、脾横波弹性成像检测。在TIPS术前,从门静脉、肘静脉、肝静脉获得样品,检测这些样品中的IL1b, IL6, IL8, IL10, IL18和γ-干扰素等水平。
研究方法:27例患者(5例急性组的患者,22例慢性组的患者)肝脏硬度增加大于10%。56例患者,肝脏硬度下降或保持不变。重要地是,全部慢性组患者,脾脏硬度降低。肝脏硬度增加的患者与肝脏硬度未增加的患者,两组患者在临床和实验室参数上没有差异。肝脏硬度增加的患者,TIPS术时,促炎细胞因子水平增高;在TIPS术后,发生器官衰竭的风险增高,生存率降低。C反应蛋白和肝硬度增加超过10%是患者发生死亡的独立预测因素。
研究结论:研究表明,系统炎症出现后,TIPS术后,患者肝脏硬度增加的风险增高;是器官衰竭和死亡的预测因素。
原始出处:
Jansen C, Moller P, Meyer C, et al. Increase in liver stiffness after transjugular intrahepatic portosystemic shunt is associated with inflammation and predicts mortality. Hepatology, 2018, 67(4), 1472-1484. doi: 10.1002/hep.29612.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#静脉#
24
#肝硬度#
34
#门静脉系#
35
#EPA#
25
#门静脉#
30