盘点:房颤指南共识一览
2016-09-19 MedSci MedSci原创
心房颤动(简称房颤)是最常见的持续性心律失常。随着年龄增长房颤的发生率不断增加,75岁以上人群可达10%。房颤时心房激动的频率达300~600次/分,心跳频率往往快而且不规则,有时候可达100~160次/分,不仅比正常人心跳快得多,而且绝对不整齐,心房失去有效的收缩功能。房颤患病率还与冠心病、高血压病和心力衰竭等疾病有密切关系。这里小M整理了2016年以来关于房颤的指南及共识与大家分享。【1】房颤
心房颤动(简称房颤)是最常见的持续性心律失常。随着年龄增长房颤的发生率不断增加,75岁以上人群可达10%。房颤时心房激动的频率达300~600次/分,心跳频率往往快而且不规则,有时候可达100~160次/分,不仅比正常人心跳快得多,而且绝对不整齐,心房失去有效的收缩功能。房颤患病率还与冠心病、高血压病和心力衰竭等疾病有密切关系。这里小M整理了2016年以来关于房颤的指南及共识与大家分享。
【1】房颤患者NOAC抗凝指南10项要点
近日,欧洲心律协会(EHRA)对2013版房颤患者非维生素拮抗剂类口服抗凝药(NOAC)实践指南进行了更新。2015年和2016年都进行了新的升级更新。新版指南内容要点如下:
1、非瓣膜性房颤是指存在机械瓣或中度至严重二尖瓣狭窄(常源于风湿性疾病)情况下发生的房颤。NOAC类实验常纳入了其他瓣膜疾病,因此瓣膜性疾病通常可以得到恰当的治疗。
2、该指南列出了一张药物间相互作用明细,这些相互作用可能影响NOAC给药。重要的药物相互作用包括抗心律失常类药物、决奈达隆(与达比加群)、利福平、HIV蛋白酶抑制剂、抗真菌药(例如伊曲康唑与酮康唑)、免疫抑制剂(环孢霉素与他克莫司,与达比加群)、抗酸剂(如PPI类)、卡马西平、苯巴比妥、苯妥英与贯叶连翘。
3、该指南还强调了从华法林治疗到NOAC的过渡策略。总体而言,由华法林转为NOAC时,应在INR≤2.0-2.5时启动NOAC治疗;而由NOAC转为华法林时,应在NOAC给药前及最后一次给药后24小时测定INR,以对华法林抗凝效果进行最好的评价。
4、在围术期抗凝管理中,不应使用低分子肝素进行桥接治疗,因为NOAC的半衰期很短。最后一次术前给药时机需考虑患者肾功能及手术出血风险。一般来说,术前24~96小时停用NOAC是合理的。
5、对于NOAC引起的出血,保守治疗对绝大多数患者而言是合理的。当发生大出血或致命性出血时,达比加群使用者可接受idarucizumab(静注5g)治疗;Xa因子抑制剂使用者应用凝血酶原复合物(50 U/kg)治疗,新药andexanet-alpha 还有待获批和上市。
6、对于进行心脏电复律的患者,可接受3周的NOAC治疗,患者无需预转化经食道超声心动图检查。
7、对于使用NOAC治疗且拟行PCI的患者,指南推荐在择期PCI术前24小时前或ACS患者入院时即停用NOAC。在PCI术后,应重新启用同种NOAC药物,并联合单抗或双抗治疗(DAPT)。接受抗凝与抗血小板治疗的患者考虑质子泵抑制剂治疗是合理。
8、在房颤患者择期PCI或发生急性冠脉综合征之后,指南建议植入裸金属支架或药物涂层支架的患者分别进行1或6个月的三联治疗(口服抗凝+DAPT)。在1或6个月之后,他们建议联合口服抗凝+阿司匹林或氯吡格雷治疗,直到PCI 1年以后。多数患者可在PCI术后1年时继续单药口服抗凝治疗。
9、对于发生过短暂性脑缺血或缺血性卒中的患者,指南建议在事件发生后1~12天内启动或重新启动OAC治疗,这取决于事件的严重性。对于颅内出血患者,如果出血原因或风险因素可以得到治疗,则应在4~8周内重新启动抗凝治疗。否则,考虑使用左心房封堵装置。
10、在处方NOAC类药物之前,需使用Cockcroft-Gault方程评估患者肾功能。严重肾功能不全患者禁行NOAC治疗(CrCl ≤15 ml/min或透析)。(文章详见——房颤患者NOAC抗凝指南10项要点)

【2】2016 CCS房颤指南更新:房颤管理
2016年9月,加拿大心血管学会(CCS)更新了房颤管理指南,加拿大心血管学会指南委员会定期更新房颤管理的新数据,本指南主要更新点有:
1.在冠状动脉疾病的各种临床表现的背景下,房产患者的抗栓治疗;
2.非维生素K拮抗剂口服抗凝药的真实数据;
3.对非维生素K拮抗剂口服抗凝药的反转用药;
4.地高辛作为速率控制剂;
5.围术期抗凝管理;
6.房颤手术治疗包括心脏术后房颤的预防和治疗。(文章详见——2016 CCS房颤指南更新:房颤管理)
【3】房颤患者合并冠心病的抗栓治疗策略与新共识解读
2016年5月27日,第十届东方心脏病学会议在上海世博园召开。大会云集了中国著名的心脏病学专家,其中浙江大学医学院附属邵逸夫医院心内科的傅国胜教授就房颤患者合并冠心病的抗栓治疗进行了策略与新共识解读,并推荐了治疗指南。(文章详见——OCC 2016:傅国胜——房颤患者合并冠心病的抗栓治疗策略与新共识解读)

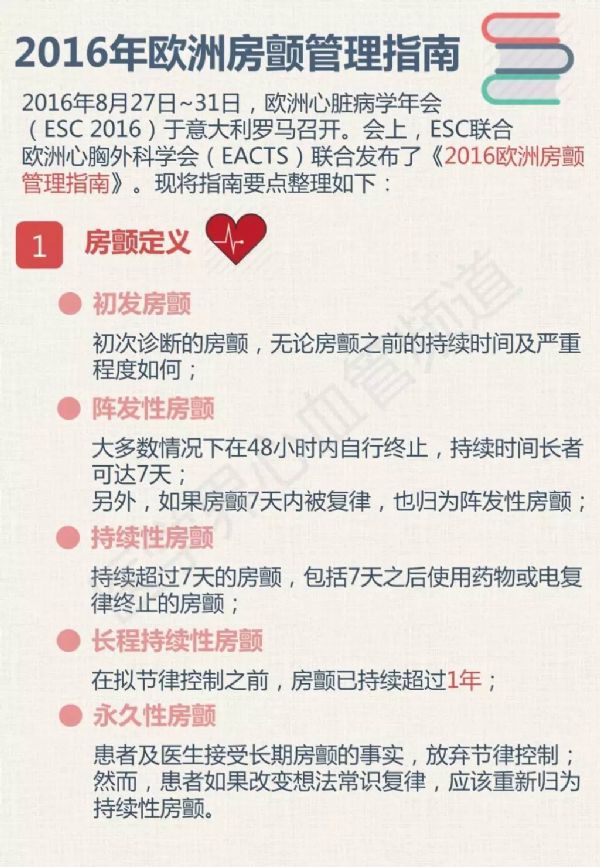
【4】2016 ESC指南:房颤的管理
2016年8月,欧洲心脏病学会(ESC)发布了房颤管理指南,为ESC第2版房颤指南,指南涉及房颤的流行病学,病理学,诊断,分类和管理等内容。(文章详见——2016 ESC指南:房颤的管理)
下面一图读懂《2016 欧洲房颤管理指南》
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







房颤的治疗因人而异,要有针对性。
40
学习啦,,,
40
值得学习
0
继续关注
37
学习了谢谢。
41
很好的内容,谢谢分享。
0