Heart:临床对瓣膜性心脏疾病的诊断报告真的准确吗?
2017-06-19 MedSci MedSci原创
常规的准确收集关于死因的信息对于公共卫生和卫生系统规划至关重要。由于临床检查对瓣膜性心脏病(VHD)的检测灵敏度相对较低,仅基于临床信息的死亡率数据可能常常低估VHD造成的死亡人数。 本研究通过对一个英国三级转诊中心中的8198名成年的死亡患者进行尸检结果和生前的临床数据信息的比对分析(平均年龄69.1岁,男性占61.3%),评估其之间的相关性。 尸检结果表明,瓣膜性心脏疾病在165名
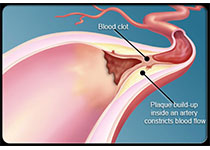
常规的准确收集关于死因的信息对于公共卫生和卫生系统规划至关重要。由于临床检查对瓣膜性心脏病(VHD)的检测灵敏度相对较低,仅基于临床信息的死亡率数据可能常常低估VHD造成的死亡人数。
本研究通过对一个英国三级转诊中心中的8198名成年的死亡患者进行尸检结果和生前的临床数据信息的比对分析(平均年龄69.1岁,男性占61.3%),评估其之间的相关性。
尸检结果表明,瓣膜性心脏疾病在165名(2.0%)死者中占主要死因,在326名(4.0%)死者中属于死因之一,在346名(4.2%)死者中占偶然死因。在瓣膜性心脏疾病占主要死因的死亡患者中,相比于尸检结果,生前的临床诊断有较高的特异性,但是敏感性低(特异性:96.8%; 95% CI 96.4%-97.2%; 敏感性:69.7%, 95% CI 62.1%-76.6%),在瓣膜性心脏疾病占死因之一的死亡患者中,特异性为98.1%; 95% CI 97.8%-98.4%; 敏感性为68.4%, 95% CI 63.1%-73.4%。通过尸检,额外地有142名(1.7%)死者的主要死因被确定为瓣膜性心脏疾病。
生前的临床诊断报告相比于尸检结果来说有较高的特异性,但是敏感性较低,这有可能低估了瓣膜性心脏病的致死率。
原始出处:
Sean C et al.Clinical information has low sensitivity for postmortem diagnosis of heart valve disease.Heart.2017 June.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#瓣膜性#
34
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
56
#ART#
31
#心脏疾病#
33
#HEART#
0
#瓣膜#
24