Cerebrovasc Dis: 无症状性实质出血史患者,静脉溶栓后脑内出血的风险未增加
2015-09-27 phylis译 MedSci原创
背景:NINDS试验显示静脉给予rtPA能够改善急性缺血性卒中的神经功能预后。排除了脑内出血(ICH)史的患者,可能是基于这类患者出血的风险增加。然而,是否应反对或支持给予先前存在ICH的患者静脉rtPA溶栓,尚不清楚。研究人员旨在通过一项回顾性基于医院单中心研究确定给予这种患者静脉rtPA溶栓的安全性。方法:研究人员总数了2006年1月到2014年4月间医院卒中中心接受静脉rtPA治疗的所有患者
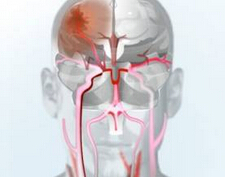
背景:NINDS试验显示静脉给予rtPA能够改善急性缺血性卒中的神经功能预后。排除了脑内出血(ICH)史的患者,可能是基于这类患者的出血风险增加。然而,是否应反对或支持给予先前存在ICH的患者静脉rtPA溶栓,尚不清楚。研究人员旨在通过一项回顾性的基于医院的单中心研究确定给予这种患者静脉rtPA溶栓的安全性。
方法:研究人员总数了2006年1月到2014年4月间医院卒中中心接受静脉rtPA治疗的所有患者的脑影像学资料,确定静脉rtPA溶栓前存在ICH。预后由NINDS试验定义的症状性ICH。
结果:共总结了640名患者脑影像学。27名患者静脉溶栓前存在ICH。仅有1名(3.7%)患者在给予静脉rtPA静脉溶栓后出现症状性ICH。剩余的613名接受静脉rtPA溶栓的患者,25名(4.1%)形成症状性ICH。
结论:回顾性研究提供了C级证据,影像学显示存在无症状性脑实质内出血的急性缺血性卒中患者,静脉溶栓后形成症状性ICH的风险没有增高。
原文出处:
AbdelRazek MA, Mowla A, Hojnacki D,et al. Prior Asymptomatic Parenchymal Hemorrhage Does Not Increase the Risk for Intracranial Hemorrhage after Intravenous Thrombolysis. Cerebrovasc Dis. 2015 Sep 25.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#静脉#
32
#Dis#
33
#脑内出血#
35
#无症状#
33
#ASC#
28