降低结直肠息肉漏诊率的新技术
2016-10-23 陈科云,刘锦涛,深圳市第八人民医院消化内科;吴进峰,深圳市第五人民医院消化内科 《中华医学杂志》
作者:陈科云,刘锦涛,深圳市第八人民医院消化内科;吴进峰,深圳市第五人民医院消化内科 结直肠癌居所有恶性肿瘤的第4位,我国目前结直肠癌的发生率和死亡率分别位于恶性肿瘤的第3和第5位,严重危害人类的健康和生命。腺瘤性息肉是结直肠癌的癌前病变,95%的结直肠癌由其发展而来。规范的肠道准备、一定的退镜时间及严格的培训等降低了息肉的漏诊率。近年来,消化内镜新技术的出现,有助于腺瘤性息肉的早
作者:陈科云,刘锦涛,深圳市第八人民医院消化内科;吴进峰,深圳市第五人民医院消化内科
结直肠癌居所有恶性肿瘤的第4位,我国目前结直肠癌的发生率和死亡率分别位于恶性肿瘤的第3和第5位,严重危害人类的健康和生命。腺瘤性息肉是结直肠癌的癌前病变,95%的结直肠癌由其发展而来。规范的肠道准备、一定的退镜时间及严格的培训等降低了息肉的漏诊率。近年来,消化内镜新技术的出现,有助于腺瘤性息肉的早发现、早诊断和早治疗,降低了结直肠癌的发生率和死亡率,综述如下。
一、电子染色内镜
1.窄带成像技术(narrow band imaging,NBI):
NBI是一种新兴的内镜技术,它采用窄带滤光器滤去了红光,留下中心波长分别为540 nm和415 nm的绿光和蓝光,由于窄波光没有覆盖所有可见光光谱,到达黏膜的深度不同,通过绿、蓝顺次成像,可得到黏膜不同层次的形态图像,提高了黏膜和黏膜下血管成像的对比度和清晰度,突出强调黏膜构造的细微改变,NBI技术联合放大内镜可更清晰、直观地显示大肠息肉样病变的轮廓、腺管开口及微血管形态,较好地区分肿瘤性与非肿瘤性病变。
Pasha等通过荟萃分析对比了高分辨NBI技术与普通高分辨结肠镜对息肉检出率的差异,发现NBI技术不能显著提高总体腺瘤检出率(OR=1.01,95%CI:0.74~1.37),2组肠镜对于扁平型息肉或直径<10 mm的息肉检出率差异无统计学意义。Sabbagh等在随后的研究中也证实了NBI技术并不能显著提高息肉检查率。Hazewinkel等则在近期一项多中心临床随机对照研究中发现NBI技术虽不能显著降低总体息肉漏诊率,但对不同病理类型的息肉,其作用不一,和普通白光结肠镜相比,NBI组的腺瘤漏诊率甚至更高,但其却能显著降低增生性息肉的漏诊率,这可能与在窄谱光源下,腺瘤及锯齿状息肉显像更暗,削弱了与周围正常黏膜组织间的颜色对比,而增生性息肉却因其良好的显像而不易被漏诊。Horimatsu等在日本的5个学术中心进行了一项前瞻性的随机对照研究,发现新一代的NBI技术有望提高息肉检出率。
2.人工智能染色技术(Fuji intelligent color enhancement,FICE):
FICE又称内镜智能分光比色技术,通过模拟色素内镜,再现黏膜表层细微结构及毛细血管走向,可更清晰地观察黏膜腺管开口的形态。Chung等研究对比了FICE技术与普通白光结肠镜,发现两者的腺瘤检出率和腺瘤漏诊率间差异均无统计学意义。Chung等也将NBI或FICE技术与普通白光结肠镜检查比较,发现不论是NBI或FICE技术均不能提高腺瘤检出率;Lapalus等则认为FICE技术虽无助于提高总体息肉检出率,但可提高远端结肠5 mm以下腺瘤性息肉的检出率,同时该研究还对比了FICE组与普通白光组检查时长,发现FICE组平均时长(27.1 min)显著高于普通白光组(18.9 min)。这无疑增加了电子染色内镜的时间成本,并有可能增加与时长相关的各种风险。
其他电子染色技术如I-Scan不仅能观察表面腺管及血管,还有针对食管、胃、肠道的模式,有研究认为其能提高息肉检出率。总之,电子染色技术作为内镜检查中的一种常用辅助功能,具有操作简单,可重复性强,无染色剂过敏等优点,在一定条件下可提高某些特定部位或类型的息肉检出率,但其更重要的功能仍是通过结合放大内镜观察黏膜腺管开口及黏膜表面微血管网,对病变的边界、形态、范围及病理性质做出初步判断。
二、自体荧光放大内镜(autofluorescence imaging videoendoscopy,AFI)
AFI根据不同组织的荧光发射光谱特征来区分病变组织,多用于早期消化道肿瘤的诊断,近年来也被尝试用来提高息肉的检出率。Matsuda等研究对比了AFI技术与普通白光结肠镜检查对息肉漏诊率的差异,发现AFI技术能显著提高右半结肠的息肉检出率,尤其是微小的平坦型息肉,但该研究仅局限于右半结肠,且样本量小,需要大规模的多中心临床研究论证。而且AFI对设备要求高,早期的临床研究结论差异较大,目前并未在临床推广应用。
三、透明帽辅助技术
透明帽是一种塑料短帽,将其安装在内镜先端后,使得镜头与消化道黏膜间可保持一定距离,提供清晰的视野和足够的空间,同时给内镜一个支点,有利于内镜前端的固定,便于进行内镜下操作,常被用于辅助止血治疗、异物取出、放大内镜检查、改善切线位和观察困难部位病变的内镜成像观察。其操作简便,并可依据病变的部位和适应证选择不同类型的透明帽。透明帽辅助肠镜(cap-assisted colonoscopy,CAC)潜在的不足之处在于肠腔内的粪便残渣易粘附在透明帽外缘,需反复冲洗和吸引才能保持良好的观察视野。
大量的研究表明,与普通肠镜相比,CAC检查可缩短插镜时间,减轻患者不适感,增加结肠肿瘤检出率,提高盲肠到达率,但其对病变检出率的作用目前仍存在争议。Rastogi等研究发现CAC检查与普通结肠镜相比,能显著提高直径≤5 mm扁平息肉的检出率(P<0.001),并可提高13%(69% VS 56%,P=0.009)的总体腺瘤检出率;Rzouq等则对427例患者进行了前瞻性的随机对照研究,他们认为CAC对锯齿状腺瘤的检出能力明显优于普通结肠镜(40例VS 20例,P=0.03),能显著提高总体锯齿状腺瘤的检出率(12.8% VS 6.6%,P=0.047),从而降低其进一步发展为大肠癌的概率。
但也有学者认为,CAC无助于提高息肉检出率,如Wijkerslooth等对比了CAC与普通结肠镜对息肉检出率的影响,共1 380例首次进行结肠镜筛查的无症状患者纳入研究,结果发现2组间的患者平均腺瘤检出数目差异无统计学意义(0.49±1.05 VS 0.50±1.03,P=0.91),认为CAC检查不能提高总体腺瘤检出率(28% VS 28%,RR=0.98,95%CI:0.82~1.16),且对于不同大小的息肉(<6 mm、6~9 mm、≥10 mm),其检出率差异亦无统计学意义。另有多项研究也得出类似的结论,认为CAC无论是对于总体息肉检出率,还是微小息肉的检出率,较普通结肠镜均无明显优势。Ng等则对16项随机对照研究进行了荟萃分析,发现CAC与普通结肠镜相比,不能提高息肉检出率(RR=1.08,95%CI:1.00~1.17);甚至有学者认为,CAC不仅无助于检出更多的病变,反而会降低息肉检出率。因此透明帽辅助对息肉检出率的意义仍需进一步研究。
四、反转技术
右半结肠具有深大的皱襞,这一特殊的解剖结构常易导致病变的漏诊,尤其是当息肉位于皱襞近端时,由于普通结肠镜视野范围有限,更易被遗漏;且右半结肠的表面积远大于远段结肠,亦可能增大病变的漏诊率。研究表明,息肉位于回盲部及升结肠是其进一步发展为大肠癌的独立危险因素。因此,若退镜时能充分观察皱襞近端的大肠黏膜,则有望提高右半结肠的息肉检出率。
结肠镜的反转技术较早应用于宽大的直肠部分,用以观察肛缘齿状线近端的病变,近期有学者尝试将这种技术应用于近端结肠以提高息肉检出率。Chandran等探讨了该技术的安全性及可行性,并对比分析了其与普通结肠镜对近端结肠息肉检出率的影响,结果显示,纳入研究的1351例患者中1295例在右半结肠实现了反转,成功率高达95.9%,无任何不良事件发生,故认为反转技术应用于右半结肠是安全、可行的,且应用反转技术对近端结肠进行二次肠镜检查时,在原有基础上再检出息肉84枚,其中75枚为腺瘤性息肉。Kim等也认为反转技术应用于近端结肠是安全可行的,并能显著提高右半结肠的息肉检出率。这提示只要肠镜前端柔软部分能达到一定的弯曲能力,就可以在观察过程中实现反转,使结肠内多部位反转检查成为可能,并通过反向观察皱襞的近端黏膜,弥补普通前视内镜视野有限的不足,提高息肉检出率。对于升结肠、直肠末段及近肛门等不易观察部位,可常规予以反转镜身以确保无病变漏诊,但应注意回盲部及直肠壶腹部情况,不可强行反转以免穿孔。
五、最新内镜技术
大多学者认为息肉的漏诊主要源于病变的位置,当息肉处于肠道弯曲部或两皱襞之间或皱褶近端方向时,则更容易被漏诊,这要求内镜医师在将肠镜送达回盲部后,退镜时应依次全面观察各肠段,尤其是皱襞后及转折处。但由于普通肠镜直视下视野有限,这类病变难免被遗漏。因此,一系列以扩大视野、铺平皱襞为目的的降低息肉漏诊率的最新内镜设备被学者们研发。
1.球囊辅助内镜(The G-EYE balloon colonoscope,endocuff-assisted colonscopy,EAC):
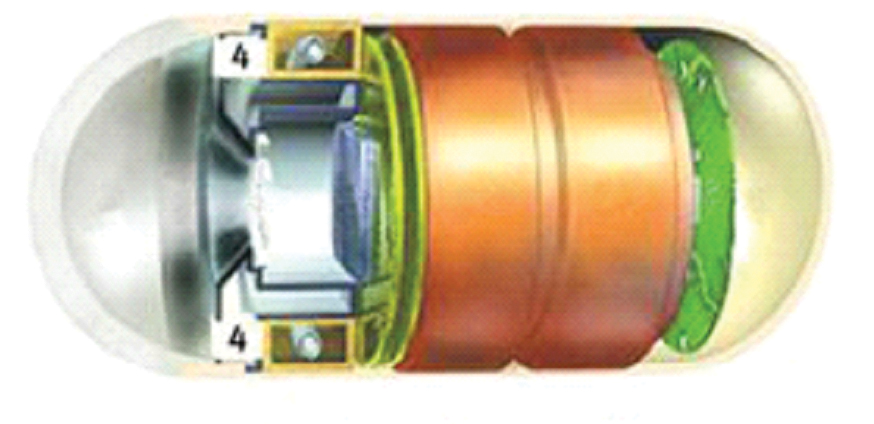
新型内镜可在结肠镜先端安装一个可调节内压的球囊,进镜时球囊处于零压力状态,退镜时使球囊膨胀,膨胀的球囊可将皱襞铺平并取直弯曲部,相对固定肠腔防止内镜在经过皱褶处时突然滑脱,球囊设有3种分压,内镜医师可根据肠腔内的情况即时调整球囊内压。Hasan等为探讨球囊辅助内镜是否能提高息肉检出率进行了一项前瞻性实验,研究由50位内镜医师在设有12枚虚拟息肉的结肠模型中完成,医师均要求在完成普通结肠镜检查后紧接着用球囊辅助内镜行第2次肠镜检查,发现球囊辅助内镜组总体息肉检出率(91.7% VS 45.8%,P<0.000 1)、显性息肉检出率(100.0% VS 75.0%,P<0.000 1)、隐藏在皱褶后的息肉检出率(88.0% VS 25.0%,P<0.000 1)均显著高于普通结肠镜。Gralnek等首次将球囊辅助内镜应用于实际临床,并对其安全性及有效性进行了评估,共47例患者纳入研究,观察指标包括达盲率、进镜及退镜时间、总操作时间、腺瘤检出率、息肉切除率,结果47例患者均成功到达回盲部,所有患者无不良反应及并发症发生,平均进镜时间4.3 min,共检出息肉44枚,息肉检出率53.2%(25/47),且息肉均被成功切除。Halpern等也在一项多中心的前瞻性随机对照研究中对比了球囊辅助内镜与普通结肠镜检查之间腺瘤检出率、腺瘤漏诊率的区别,发现球囊辅助内镜的腺瘤检出率显著高于普通结肠镜(40.4% VS 25.9%,P=0.115);并能降低腺瘤漏诊率(7.5% VS 44.7%,P=0.0002)。因此,这类球囊辅助内镜在实际操作中是安全可行的,对提高息肉检出率的作用也是肯定的。
类似的辅助工具还包括一种侧边有很多柔软指状突出物的球囊类似物(endocuff-assisted colonscopy,EAC),检查时同样只需将其安装在内镜先端部即可,但不同于普通透明帽的是,它前端不需突出于镜身,对吸引及活检孔道元任何影响,且可以通过突出于侧边的弹性指状物相对固定视野,有利于更好的观察皱襞及肠道弯曲部。Pioche等对32位不同级别的内镜医师在设有13枚模拟息肉的结直肠模型中探讨了其对息肉检出率的影响,结果发现,EAC检出的病变数显著高于普通结肠镜(9.9 VS 7.5,P=0.03);且在调整相关影响因素后,发现EAC能在普通结肠镜的基础上检出额外的1.2枚息肉(P=0.0037)。但该辅助工具尚未应用于临床,其安全性及可行性有待进一步研究。
2.广角结肠镜:
目前大多数的结肠镜都是140°视野,只有一家厂商拥有170°视野结肠镜(wide-angle colonoscopy,WA colonoscopy)。East等用CTC软件模仿了普通结肠镜与这种170°广角结肠镜所见黏膜面积间的差异,发现用140°视野角度观察时,可见全大肠面积的85%左右,而当用170°视野角度观察时,所见大肠面积明显增加,仅约7%肠黏膜无法看见。在实际应用中,这种广角肠镜对于各种疾病的检出率、漏诊率仍是有争议的。Deenadayalu等发现这种增加肠镜视野角度并不能提高息肉检出率;Fatima等则认为,虽然170°广角肠镜无助于提高息肉检出率,但和普通结肠镜相比,能显著缩短进镜和退镜时间。
另一种新型广角肠镜(extra-wide-angle-view colonscope)其内镜先端部的镜头凸出于镜身,除普通结肠镜原有的140°前视镜头外,同时还设有一个拥有144°~232°视野的侧视镜头,明显扩大了观察范围。Uraoka等在设有16枚模拟息肉(其中8枚隐藏在皱褶后)的结直肠模型中探讨了其对病变检出率的效用,共32位内镜医师参与实验,结果显示广角肠镜能显著提高总体息肉检出率(68% VS 51%,P<0.0001),且对于隐藏在皱褶后的息肉检出率,广角肠镜也显著高于普通结肠镜(61.7% VS 46.9%,P=0.0009)。有学者在随后的临床应用中对广角肠镜进行了安全性及可行性分析,纳入研究的47例患者均成功到达回盲部,平均进镜时间(6.4±4.9)min,无不良事件发生;共检出47枚息肉,28枚腺瘤性息肉,其中29枚(61.7%)息肉、16枚(57.1%)腺瘤性息肉是在首次进行的广角肠镜中被检出,因此,Uraoka等认为广角肠镜是安全可行的,并有望提高息肉检出率。
3. "第三只眼"反转肠镜(Third eye retroscopy,TER)、"第三只眼"全景肠镜(Third eye panoramic,TEP):
TER是一个小型独立的内镜装置,可安装在肠镜辅助通道中,当其头部伸出肠镜前端后能实现180°反转观察肠黏膜,弥补了标准肠镜无法观察皱襞后壁及肠道弯曲部的病变这种不足,降低息肉漏诊率。Leufkens等对比了使用TER装置与普通结肠镜对息肉检出率的影响,发现使用TER组能提高约23%的腺瘤检出率(45.8% VS 22.6%);Siersema等在随后的研究中也得出类似的结论,发现TER组总体腺瘤检出率较普通结肠镜可提高23.2%。
然而TER占用肠镜设备孔道,一旦发现息肉,必须拿出TER放入治疗设备,然后再重新置入TER,这种操作显得繁琐,且延长了操作时间。Leufkens等证实了使用TER的平均退镜时间比普通结肠镜更长(7.58 min VS 9.52 min,P<0.001),总操作时长为(16.97 min VS 20.87 min,P<0.001)。为克服该缺陷,Rubin等在2014年的消化疾病周上引进了一种被称之为TEP的新型设备,它是一个独立小型的内镜装置,可安装在内镜先端部的外侧缘,其左右两侧带有的摄像头可在退镜时观察到两侧的大肠黏膜,既扩大了观察视野,又不需占用活检孔道。但这3个视野均为相对独立视角,所以在检查过程中需3个独立的显示器分别进行显示,这就要求检查者在肠镜检查手法和观察习惯上有所改变,或增加观察人员。其对息肉检出率的意义有待进一步研究。
4.330°全周肠镜(full-spectrum endoscopy,FUSE):
这种最新的内镜设备结合了140°前置视野和双侧135°反转视野(就如同侧方2个第3只眼反转肠镜)可获得330°环周视野,显著提高息肉检出率。Ron-Tal等首次在结直肠模型中(包含21枚模拟息肉)探讨了FUSE对息肉检出率的意义,37名从未使用过FUSE的内镜医师纳入研究,医师均先后行普通结肠镜、FUSE,结果普通结肠镜组平均检出息肉(11.1±2.3)枚,FUSE组平均检出息肉(18.0±1.9)枚,FUSE组的总体息肉检出率显著高于普通结肠镜组(85.9% VS 52.9%,P<0.001),且对于隐藏在皱襞后的息肉检出率,FUSE的作用更为明显(81.9% VS 31.9%,P<0.0001)。Gralnek等在随后的研究中对比分析了FUSE与普通结肠镜对息肉检出率的差异,A组(88例)先行普通结肠镜紧接着行FUSE检查,B组(97例)则调换检查顺序,结果显示B组中FUSE的腺瘤漏诊率7.5%(5/67)低于A组普通结肠镜的息肉漏诊率40.8%(20/49),差异有统计学意义。FUSE的3个视野均为相对独立视角,在检查过程中亦需3个独立的显示器,同样要求检查者在肠镜检查手法和观察习惯上有所改变,或增加观察人员。
总之,结直肠息肉的漏诊在结肠镜检查中普遍存在,加深对息肉漏诊危险因素的认识及探索降低息肉漏诊率的有效手段临床意义重大。我们在前期的回顾性多因素回归分析中发现漏诊率与息肉大小、形态、基础息肉数相关。当然,这些客观因素我们无法掌控,但通过改进肠道准备质量、提高达盲率、保证足够退镜时间并结合具体情况尝试使用透明帽、电子染色、反转技术、广角全景肠镜技术等有望提高结直肠息肉的检出率,将息肉漏诊率降至最低。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#新技术#
27
很好,不错,以后会多学习
61
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
53
学习并分享了
44
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
45
#漏诊#
22
#结直肠#
23
#结直肠息肉#
35