Sci Rep:基于脉冲调制AML光纤激光器的人体视网膜成像系统新方法
2019-01-17 MedSci MedSci原创
韩国光州科学技术研究院先进光子学研究所的Lee HD和韩国大学医学院眼科的Lee B等人近日在Sci Rep杂志上发表了一篇重要的研究论文,在这项研究中,他们将1080nm波长的脉冲调制AML光纤激光器作为OCT系统的动态扫描源,用于人体视网膜体内成像。
韩国光州科学技术研究院先进光子学研究所的Lee HD和韩国大学医学院眼科的Lee B等人近日在Sci Rep杂志上发表了一篇重要的研究论文,在这项研究中,他们将1080nm波长的脉冲调制AML光纤激光器作为OCT系统的动态扫描源,用于人体视网膜体内成像。
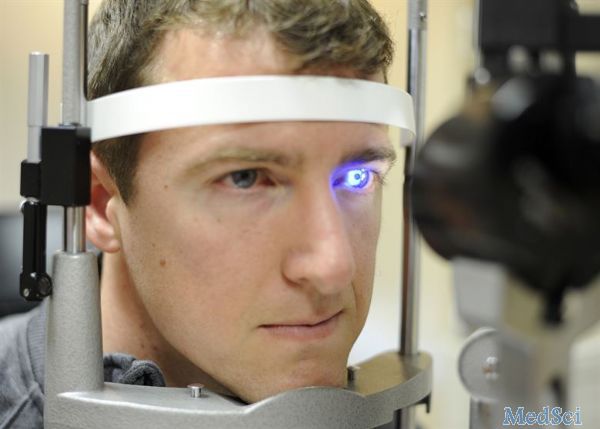
光学相干断层扫描(OCT)是一种非侵入性的成像模式,可以提供组织的高分辨率横截面图像。特别是在视网膜成像中,OCT已成为诊断眼病的更有价值的成像工具之一。考虑到眼睛的散射和吸收等特性,首先选择1000nm OCT系统用于视网膜成像。
动态AML波长扫描光纤激光器采用偏光纤构成,无需缓冲方法,平均线宽为0.625nm,光谱带宽为81.15nm,占空比为90%。他们使用所提出的OCT系统成功地获得了人类视网膜体内图像,没有额外的k时钟,同时可以提供43.1°的宽视场影像。使用该OCT系统,可以将主视网膜层(例如视网膜色素上皮)与OCT图像区分开,轴向分辨率为6.3μm。
原文出处:
Lee, H.D., et al., Akinetic swept-source optical coherence tomography based on a pulse-modulated active mode locking fiber laser for human retinal imaging. Sci Rep, 2018. 8(1): p. 17660.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#新方法#
0
#视网膜#
24
#激光#
27