Diabetologia:一项对来自芬兰4组11,896名年轻人的前瞻性研究:循环代谢物与2型糖尿病的风险?
2019-12-28 MedSci MedSci原创
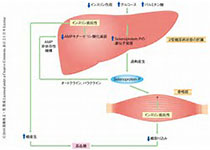
代谢组学技术已经在中老年个体的病例对照研究中发现了许多2型糖尿病风险的血液生物标志物。我们的目的是验证现有的代谢生物标志物,并在大量的年轻人中发现预测未来糖尿病的新生物标志物。
代谢组学技术已经在中老年个体的病例对照研究中发现了许多2型糖尿病风险的血液生物标志物。我们的目的是验证现有的代谢生物标志物,并在大量的年轻人中发现预测未来糖尿病的新生物标志物。
研究人员采用核磁共振代谢组学来自芬兰4个观察组(基线年龄24-45岁)的11896名个体的229个循环代谢测量进行量化。在8-15年的随访中(392例病例),根据性别、年龄、BMI和空腹血糖。对基线代谢物与患糖尿病风险之间的关系进行了校正。
研究结果显示,在229项代谢指标中,113项与4组患者的2型糖尿病发病相关(or每1 SD:
0.59-1.50;p < 0.0009)。糖尿病风险最强的生物标志物是VLDL颗粒中的支链和芳香氨基酸(或1.31-1.33)和三酰基甘油(或1.33-1.50),以及大HDL颗粒中的亚油酸n-6脂肪酸(或0.75)和非酯化胆固醇(或0.59)。代谢生物标志物与负荷后葡萄糖和胰岛素抵抗的恶化比与未来空腹高血糖更密切相关。多代谢物评分包括苯丙氨酸、大HDL中的非酯化胆固醇以及大VLDL中胆甾酯与总脂质的比率与其中一个队列(平均年龄31岁)中未来的糖尿病风险(OR10.1比较多代谢物评分中的较高和下五分之一的个体)相关。
研究结果表明,通过多个分子途径的代谢生物标志物已经可以预测年轻人患糖尿病的长期风险。全面的代谢谱分析可能有助于针对风险增加的年轻无症状个体采取预防措施。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#前瞻性#
20
#DIA#
17
#代谢物#
23
#BET#
27
#前瞻性研究#
25
谢谢MedSci提供最新的资讯
42