2018 ESMO:立足实践,Nivolumab真实世界研究与临床试验结果遥相呼应
2018-10-29 佚名 肿瘤资讯
2018年欧洲肿瘤内科学会(ESMO)年会在德国慕尼黑(Munich)举行,ESMO年会是欧洲最负盛名和最有影响力的肿瘤学会议,在世界上享有盛誉。本届ESMO年会的主题是“Securing access to optimal cancer care”。一如既往,在晚期NSCLC领域,免疫治疗的进展仍是当红花旦。
2015年,纳武利尤单抗获得美国FDA批准用非小细胞肺癌(NSCLC),今年6月,纳武利尤单抗在中国获批用于经治晚期NSCLC患者。作为全球首个取得晚期NSCLC治疗适应症的PD-1单抗,纳武利尤单抗在国际上临床应用于NSCLC迄今已3年有余,其在真实世界中的疗效和安全性如何?是否与临床试验结果相互印证呢?在本次的ESMO大会上,多项研究报道了纳武利尤单抗用于真实世界的疗效和安全性。
1469P EVIDENS研究:一项来自法国真实世界的观察性研究,评估1394例患者接受纳武利尤单抗治疗晚期NSCLC的初步结果
EVIDENS研究是一项观察性、多中心、纵向队列研究,旨在评估法国真实世界接受纳武利尤单抗治疗NSCLC患者的临床特征,并分析其疗效和安全性。该研究筛选了从2016年12月至2017年11月,来自法国146个研究中心的1462例肺癌患者。其中1394例NSCLC患者接受纳武利尤单抗治疗,自患者接受纳武利尤单抗治疗开始随访36个月。本次分析的人群,最短的随访时间和中位随访时间分别为8个月和11.5个月。
其中鳞癌和非鳞癌NSCLC患者分别为434例(31.1%) 和960例(68.9%)。研究基线的患者特征与晚期NSCLC总体人群的特征相似:中位年龄为66岁(范围:35-91岁),男性占69.2%,当下和既往吸烟者占89.6%,PS 0-1分的占83.2%,279 (20.0%)例患者合并脑转移,41例(2.9%)有活动性自身免疫性疾病。187例患者进行了PD-L1表达检测,其中121 (64.7%)患者的PD-L1表达≥1%。828例非鳞NSCLC患者进行了EGFR突变检测,46例(5.6%) 携带EGFR突变;752例非鳞NSCLC患者接受ALK重排检测,6例(0.6%)携带ALK重排。纳武利尤单抗用于一线、二线或≥三线治疗的患者分别占0.6%、74.0%和25.4%。
此次发表的研究结果显示:治疗6个月,研究者评估纳武利尤单抗治疗最佳缓解率为16.5%(部分缓解率15.6%和完全缓解率0.9%)。非鳞和鳞癌NSCLC患者接受纳武利尤单抗治疗的中位OS分别为11.0和9.2个月;6个月的OS率分别为65.0%和66.0%。自入组开始计算,非鳞和鳞癌NSCLC患者接受纳武利尤单抗治疗的中位PFS均为2.8个月;治疗6个月的PFS率分别为31.2%和28.9%。
1394例患者中,治疗相关的不良事件(TRAEs)发生率为31.6%(440例),3-4级TRAEs发生率为7.0%(98例),出现TRAEs的中位时间为0.62个月,因TRAEs导致永久停药的患者占4.2%(59例)。未出现治疗相关性死亡病例报告。
任意级别最常见的TRAEs(>=1%)包括:无力(5.4%)、腹泻(3.8%)、瘙痒(3.2%)、甲亢(2.7%)、甲减(2.2%)、关节痛(2.2%)、疲劳(1.6%)、食欲减低(1.5%)、贫血(1.3%)和皮疹(1.0%)。免疫相关的TRAEs发生率为12.2%,其中3-4级免疫相关TRAEs发生率为1.4%。任意级别间质性肺炎的发生率为0.9%(12例),结肠炎发生率为0.6%(8例)、心功能异常发生率为0.1%(2例)。11例(1.6%)患者报道神经系统异常,头痛和感觉异常均为7例(0.5%)。
EVIDENS研究是在法国进行的最大样本量的研究,评估纳武利尤单抗用于真实世界肺癌患者的疗效。EVIDENS研究除了患者的PS评分状态外,患者的其他特征(如年龄、性别、吸烟状态)均与既往研究报道的纳武利尤单抗全球III临床试验CheckMate 017研究 和CheckMate 057 研究中的患者特征一致。其初步结果确认了纳武利尤单抗在真实世界临床实践中用于晚期NSCLC二线及以上治疗的疗效和安全性,研究的人群中包括既往临床试验中未纳入的患者群体,更能真实的反映晚期NSCLC患者的全貌。后续将会报告生活质量评估的结果,将可以更好的评估NSCLC患者从纳武利尤单抗治疗中的获益。
1217P 纳武利尤单抗治疗NSCLC日本真实世界临床实践中的安全性分析:上市后全案例监测的中期摘要
纳武利尤单抗2015年12月在日本获批用于二线治疗经治不可切除、晚期或复发性NSCLC。基于日本药品监管部门在批准上市时的审核要求进行上市后研究,即从2015年12月17日至2016年3月31日,日本所有接受纳武利尤单抗治疗的患者均进行登记并随访1年,旨在进一步评估纳武利尤单抗用于真实世界中的安全性。该研究遵循日本上市后实践研究规定进行,采用病例报告表(CRFs)的形式收集安全性数据。
中期分析结果基于截至2018年1月3日上交CRFs的患者数据总结。研究期间内共入组3808例患者,至截止日期共收集了3612份CRFs,疗效分析纳入其中的3381例患者,1年生存率为42.38% (1433/3381;95% CI:40.71-44.07)。
安全性分析纳入了其中的3606例患者,患者特征包括:男性占72.0%(2595/3606),平均年龄为65.7岁,其中>=65岁的患者占62.5%(2253/3605), 77%的患者ECOG PS 评分为0-1分 (2796/3603%);腺癌和鳞癌患者比例分别为66.0%(2380/3606)和28.4%(1023/3606)。接受纳武利尤单抗作为一线、二线、三线或以上治疗的患者比例分别为0.8%、20.8%和78.2%,纳武利尤单抗的平均治疗时间为8个周期。
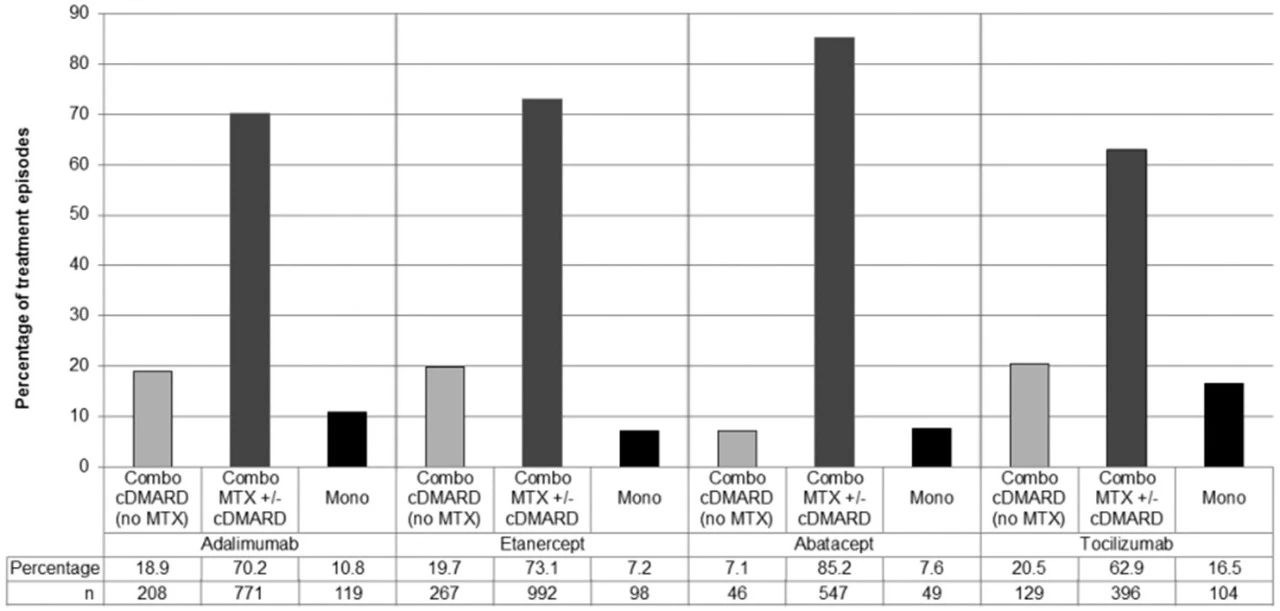
安全性分析结果显示:任意级别的与药物治疗相关不良反应(ADRs)发生率为46.8%(1688/3606)。研究者根据发生ADRs的器官系统对其进行分类汇总。最常见的ADR包括间质性肺炎、甲状腺功能减低、腹泻、发热、输液反应、AST升高和乏力,总结请见下表。
特别关注的不良事件(包含药物相关不良反应)有间质性肺病(ILD,9.57%),甲状腺功能异常(9.04%),肝功能异常(7.93%),输液反应(5.57%) 和结肠炎/严重腹泻(5.57%),详见下图,研究根据患者从接受纳武利尤单抗到出现间质性肺炎的中位时间进行了分析,大多数患者出现在用药后1-2个月内。同时采用Fine and Gray比例风险模型进行单因素和多因素分析出现ILD的危险因素。多因素分析显示,ILD的危险因素包括胸部CT除肺癌以外的异常表现、既往或合并ILD。
综上,该研究中期结果显示,在经治不可切除晚期或复发性日本NSCLC患者中,除间质性肺炎外,纳武利尤单抗显示出与临床研究相似的安全性。这一结果也进一步印证了纳武利尤单抗的疗效和安全性,为真实世界中的使用提供了更有力的证据。
1468P GECP 1605/NIVEX研究:西班牙EAP项目纳武利尤单抗用于真实世界经治晚期NSCLC患者的治疗经验
NIVEX研究旨在评估纳武利尤单抗在西班牙真实世界临床实践的疗效和安全性。研究纳入分析了来自西班牙EAP项目665例经治NSCLC患者,包括从2015年1月开始接受治疗的鳞癌和2015年6月开始接受治疗的非鳞癌患者,截至到2017年11月,至少接受一剂纳武利尤单抗治疗。
纳入分析的患者中位年龄为61岁(32-85),男性占73.1%,ECOG评分 0-1分的患者占比85.1%,当下或既往吸烟者占88%;合并骨转移,肝转移和脑转移的患者分别占34.7%,20.6%和15.3%;鳞癌和非鳞癌NSCLC患者分别为128例(19.2%)和537例(80.8%);7%的患者携带EGFR突变。在进行PD-L1表达检测的患者中,PD-L1表达≥1%的患者占33%。接受纳武利尤单抗治疗前接受过1线、2线和≥3线的患者分别为35.9%、33.7%和30.4%。
研究中位随访时间8.2个月,中位OS为8.97个月(95% CI:7.69-10.24),中位PFS为3.23个月(95% CI:2.77-3.70)。预计1年OS率和PFS率分别为42.4% (95%CI:38.5-42.8%)和22.2% (95% CI:19.1-25.3%)。其中,二线接受纳武利尤单抗治疗的患者,中位OS为10.3个月(95%CI:8.2-12.3);三线接受纳武利尤单抗治疗的患者,中位OS为8.2个月(95% CI 6.2-10.2),不同组织学类型的患者未观察到PFS或OS的差异。
安全性方面,接受纳武利尤单抗治疗的患者,296例 (44.5%) 报道有不良事件(AE)发生,69例(10.4%)患者出现≥3级AE。根据患者是否出现≥3级AE分析OS,出现或未出现≥3级AE的患者,中位OS分别为13.1个月(95%CI:10.63-15.57)和6.03个月(95%CI:4.76-7.31),P<0.001。
目前纳武利尤单抗已是各大指南推荐的晚期NSCLC二线治疗标准治疗方案。NIVEX研究结果同样证实了在真实世界临床实践中,纳武利尤单抗的疗效和安全性与既往临床试验报道一致,再次确立了纳武利尤单抗在真实世界中NSCLC治疗的地位。且如上图所示,出现任意级别AE的患者OS更长,特别是治疗中出现≥3级AE的患者,中位OS时间明显延长,同时提示其治疗过程中于AE发生可能预示更好的OS获益趋势。
总结
上述三项研究分别报告了纳武利尤单抗在法国、日本和西班牙用于真实世界临床实践中的疗效和安全性,其结果一致证实,纳武利尤单抗用于真实世界临床实践同样可以取得与临床试验相似的结果和安全性,未观察到预期以外的不良事件。这些真实世界的研究数据,为在更广泛的NSCLC患者中应用提供了纳武利尤单抗的疗效和安全性验证数据,进一步确立了其作为晚期NSCLC二线治疗标准治疗方案的地位。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#SMO#
20
#遥相呼应#
34
#NIV#
31
#mAb#
21
#ESMO#
24
#真实世界#
25