ACC 2018:两种降压药物或增死亡风险,血压波动大注意调整药物
2018-03-16 文韬 中国循环杂志
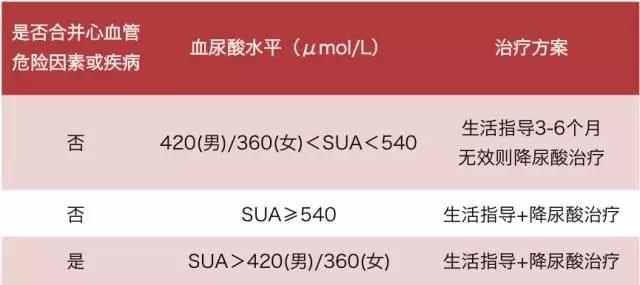
2018 年美国心脏病学会(ACC)学术年会上,美国Clements等报告,使用α受体阻滞剂和中枢性α- 2受体激动剂降压治疗的患者血压变异性增加,从而可能会增加死亡风险。
作者建议,这两种药物不应用于降压治疗。
研究人员分析了2007年1月到2011年12月间入选ALLHAERT研究的10903名高血压患者,每人至少测量了七次血压,并记录了这些患者的降压药物。
研究发现应用α受体阻滞剂和中枢性α-2受体激动剂的患者血压变异性较高。
血压变异性是指患者在一定时间内血压波动的程度。血压变异性按照观察时间的长短可分为短时变异性和长时变异性。
短时变异性指24小时内同次就诊血压变异和昼夜血压的变化。长时血压变异性是指数日间变异(家庭自测血压变异)、数周间变异(随诊间血压变异)和数月甚至季节间血压变异等。
在Clements等的另一项研究中,作者将诊室血压变异程度(OBPV)分为<13.3、13.3~16.4、16.4~19、19-22.7和>22.7 mmHg五组。
结果发现,诊室血压变异程度越大,患者的死亡率越高。
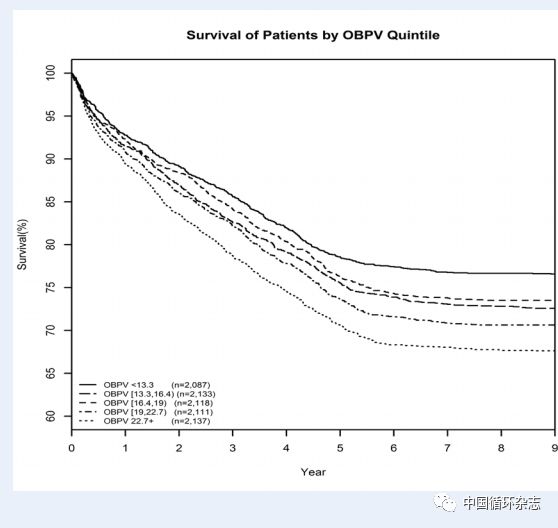
作者表示,如果患者血压波动比较大,应与医生沟通,更换降压方案。
也有研究证明,短期和长期血压变异性增加,均与心脑血管事件和全因死亡独立相关,随诊期间血压变异性是心血管事件强预测因素,其作用独立于平均血压之外。
原始出处:
[1]New Definitions of Visit-to-Visit Office Blood Pressure Variability and its Effect on All-Cause Mortality. ACC 2018.
[2]Does Office Blood Pressure Variability Predict Mortality Among Antihypertensive Classes.ACC 2018.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#血压波动#
31
#死亡风险#
38
#降压#
25
#ACC#
30
学习了.谢谢分享
71