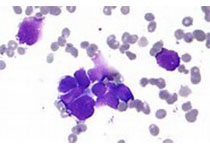
Blood:CLL细胞会损害CD8+ T细胞的线粒体适应性、降低CAR T细胞疗法疗效!
2019-05-16 Qinqiyun MedSci原创
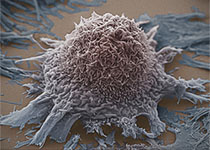
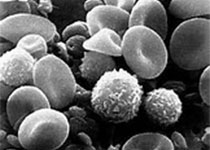
在慢性淋巴细胞白血病(CLL)中,获得性T细胞功能缺陷的机制尚未明确,极大阻碍了T细胞免疫疗法的发展。Jaco A. C. van Bruggen等人既往发现,在受到刺激后,CLL中的CD8+ T细胞表现出激活受损和葡萄糖摄取减少。CLL患者的CD8+ T细胞长期暴露于白血病B细胞的环境下,可能会影响代谢稳态,从而导致受刺激时发生异常的代谢重编程。现Jaco等人再次在CLL中,静止的CD8+ T细
现Jaco等人再次在CLL中,静止的CD8+ T细胞的细胞内GLUT1的储备减少,而且线粒体代谢谱发生改变,如线粒体呼吸、膜电位和活性氧水平均增加。与此同时,PGC-1α水平降低,CLL患者来源的CD8+ T细胞受刺激后的线粒体生物发生受损。
为了寻找这些发现的治疗相关性,研究人员分析了CLL患者输注CD19定向嵌合抗原受体(CAR)前CD8+ T细胞的线粒体发生;发现与无缓解的患者相比,在随后完全缓解的病例中,输注的CD8+ CAR T 细胞增加了线粒体质量,这点与CAR T细胞扩张和持久性呈正相关。
综上所述,Jaco A. C. van Bruggen等人的研究提示在CD8+ T 细胞中,GLUT1储备和线粒体适应性均受损。因此,增强CAR T细胞的线粒体发生或可提高CAR T细胞疗法等新兴细胞免疫疗法的疗效。
Jaco A. C. van Bruggen, et al.Chronic lymphocytic leukemia cells impair mitochondrial fitness in CD8+ T cells and impede CAR T cell efficacy. Blood 2019 :blood.2018885863; doi: https://doi.org/10.1182/blood.2018885863
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#T细胞疗法#
28
#CD8#
0
#适应性#
31
谢谢梅斯提供这么好的信息,学到很多
34