厦门大学夏宁邵团队发表新型乙肝治疗性疫苗的研究成果
2019-03-31 佚名 厦门大学
3月29日,国际权威胃肠肝病期刊Gut(JCR1区、IF 17.0)在线刊出了厦门大学夏宁邵教授团队发表的题为“A unique B cell epitope-based particulate vaccine shows effective suppression of hepatitis B surface antigen in mice”的研究论文。该研究发展了一种新型的B细胞表位嵌合型类病
3月29日,国际权威胃肠肝病期刊Gut(JCR1区、IF 17.0)在线刊出了厦门大学夏宁邵教授团队发表的题为“A unique B cell epitope-based particulate vaccine shows effective suppression of hepatitis B surface antigen in mice”的研究论文。该研究发展了一种新型的B细胞表位嵌合型类病毒颗粒乙肝治疗性疫苗,在多种体内外模型中证实了其对慢性乙型肝炎病毒(HBV)感染的治疗潜力,为研发治疗慢性乙肝的原创药物提供了新思路。
乙肝预防性疫苗显着减少了HBV新发感染,但目前全球仍有约2.5亿慢性HBV感染者,若未及时得到有效治疗,可能发展为肝癌、肝硬化等终末期肝病并导致死亡。我国慢性乙肝疾病负担较为严重,据估算目前有7000余万慢性HBV携带者,约2800万慢性乙肝患者,因乙肝死亡的人数占全球的近50%。实现HBV表面抗原(HBsAg)血清学阴转或血清学转换是慢性乙肝治疗的理想终点,但当前的药物较难实现该目标。慢性乙肝患者体内高水平的HBsAg是导致免疫耗竭(耐受)进而使感染迁延不愈的重要原因,通过有效抑制HBsAg并持续一定的时间,有望重建HBsAg特异的B细胞和T细胞应答,进而提高临床治愈率。针对慢性乙肝的新药研发竞争激烈,治疗性疫苗是其中一类颇有前景也充满挑战的生物制品。
目前在研的乙肝治疗性疫苗多数基于诱导T 细胞免疫应答设计或采用完整病毒蛋白或短肽作为免疫原,但在慢性HBV感染者外周循环存在高水平病毒抗原(如HBsAg)的情况下,针对优势表位的特异性免疫细胞常处于耗竭/失能状态,难以实现预期的临床疗效。因此,研制乙肝治疗性疫苗,需要进一步拓展思路。
夏宁邵教授团队在前期对Anti-HBs单抗盘的性质及其体内外生物学功能的研究中发现,抗体除具备经典的病毒中和作用以外,还能通过Fc介导的调理作用高效清除循环中的HBsAg;更为重要的是,抗体介导病毒抗原清除的能力依赖于其识别的表位,受识别表位决定的抗原抗体免疫复合物结构特征使得并非所有识别HBsAg的抗体都具有显着的治疗活性。通过功能抗体靶向筛选技术,确定了识别非免疫优势sA表位的E6F6抗体在动物体内具有持久有效的HBsAg清除功能(Gut,2016),提示sA表位可能成为新型乙肝治疗性疫苗的效应靶标,申请的相关核心发明专利已获美国、日本、加拿大、澳大利亚和韩国授权。有鉴于此,该团队另辟蹊径,提出在具有免疫增强功能的颗粒蛋白载体上展示E6F6单抗所识别的sA表位从而构建B细胞表位嵌合型类病毒颗粒疫苗的设想,期望该疫苗能在机体中诱导具有治疗功能的抗体应答。
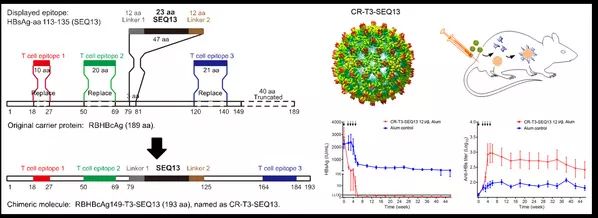
在该研究中,团队基于蹄蝠肝炎病毒衣壳蛋白优化改造出一种新型类病毒颗粒免疫增强载体CR-T3。该载体有显着的免疫增强作用,能在免疫耐受个体中诱导体液/细胞免疫应答。将sA表位移植至CR-T3载体上,获得了成功展示sA表位的CR-T3-SEQ13候选治疗性疫苗分子。CR-T3-SEQ13可在HBV转基因小鼠、HDI-HBV小鼠等多种HBV持续携带动物模型中刺激机体产生识别sA表位的类E6F6抗体,进而有效降低各模型小鼠体内HBsAg、HBV DNA水平;在非人灵长类动物模型中,CR-T3-SEQ13能诱导食蟹猴产生高滴度的sA表位抗体,其免疫后多抗血清通过被动免疫可有效清除HBV携带小鼠体内的病毒。目前,该团队正在积极推进CR-T3-SEQ13乙肝治疗性疫苗向临床转化。
厦门大学博士后张天英、博士生郭雪染和博士生巫洋涛为该论文共同第一作者,夏宁邵教授、袁权副教授、张军教授为该论文的共同通讯作者。该研究获得了“艾滋病和病毒性肝炎等重大传染病防治”科技重大专项、国家自然科学基金等项目资助。
原始出处:Zhang TY, Guo XR, Wu YT, et al. A unique B cell epitope-based particulate vaccine shows effective suppression of hepatitis B surface antigen in mice. Gut. 2019 Mar 29.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#厦门#
39
#研究成果#
0
好
74
学习了谢谢分享
1
学习了很有用不错
71
学习学习学习
79