AANS 2016:椎管狭窄使用棘突间固定装置与采用减压术的效果相当
2016-05-08 MedSci MedSci原创
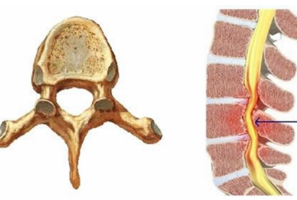
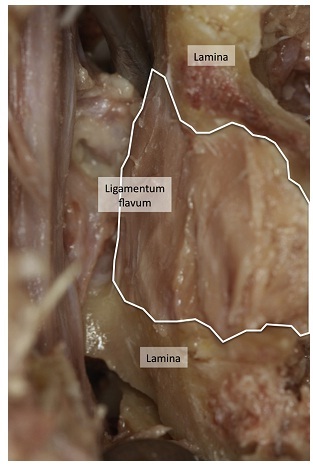
AANS 2016:椎管狭窄使用棘突间固定装置与采用减压术的效果相当据美国神经外科医师协会(AANS)2016年会上的一项新的研究报道显示,使用棘突间固定装置来治疗退行性腰椎管狭窄伴神经源性间歇性跛行是安全的,且效果与减压术的效果相似。Bernhard Meyer博士在会议上说道,“治疗后24个月的结果显示,Aperius的效果并不差于标准减压术的治疗效果。而且手术创伤很小,但是24个月患者再次手
Bernhard Meyer博士在会议上说道,“治疗后24个月的结果显示,Aperius的效果并不差于标准减压术的治疗效果。而且手术创伤很小,但是24个月患者再次手术率较高。”
在此多中心前瞻性临床试验种,研究人员共纳入了163名患者,随机分为棘突间固定装置(IPD)经皮插入治疗组和减压术治疗组。研究对象来自于来自欧洲的19个地区,平均年龄为65±11岁。评估患者的身体功能、症状严重程度和患者的满意度,直至治疗后24个月。使用VAS评分来评估患者腿、臀部、腹股沟和背部的疼痛状况,并使用第2版本的SF-36调查问卷确定患者的生活质量。
结果发现,基线至治疗后12个月,两组患者的平均身体功能改变下降程度均等,且在24个月时达到稳定。与减压术组患者相比, IPD组患者的手术时间较短,出血较少。两组患者的症状严重程度及VAS腿痛评分均得到了改善。IPD组患者再次手术率为18%,而减压术组为11%。
该研究结果证实了其他三个在欧洲进行的随机临床试验的研究结果。但是,Meyer表示,其治疗的后果仍存在不明确的地方。
原始出处:
Kristine Houck. Similar results seen with use of interspinous process device vs decompression for lumbar spinal stenosis. Healio, May 4, 2016.
Meyer B, et al. Paper #622. Presented at: American Association of Neurological Surgeons Annual Meeting. April 30-May 4, 2016; Chicago.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#椎管#
24
#椎管狭窄#
27
值得学习
101
#AAN#
27