Diabetic Med:葡萄糖警报系统可改善健康专业人员对不良血糖的反应,并减少非重症监护住院患者的高血糖发作次数
2018-10-24 MedSci MedSci原创
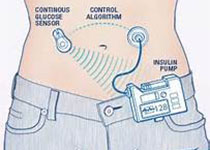
近日,国际杂志 《Diabetic Med》上在线发表一项关于葡萄糖警报系统可改善健康专业人员对不良血糖的反应,并减少非重症监护住院患者的高血糖发作次数的研究。研究目的是调查新型葡萄糖警报系统的效果,包括墨尔本葡萄糖警报途径和具有葡萄糖警报功能的网络血糖仪,以用于护理和医院医务人员对不良血糖的反应。 研究人员在三级医院的非重症监护病房进行在4个月(n=148或660患者-日)的前瞻性,前后
近日,国际杂志 《Diabetic
Med》上在线发表一项关于葡萄糖警报系统可改善健康专业人员对不良血糖的反应,并减少非重症监护住院患者的高血糖发作次数的研究。研究目的是调查新型葡萄糖警报系统的效果,包括墨尔本葡萄糖警报途径和具有葡萄糖警报功能的网络血糖仪,以用于护理和医院医务人员对不良血糖的反应。
研究人员在三级医院的非重症监护病房进行在4个月(n=148或660患者-日)的前瞻性,前后观察研究。干预措施包括两个组成部分,旨在促进健康专业人员对血糖测量的一致反应:(1)临床升级途径,墨尔本葡萄糖警报途径,以及(2)联网血糖仪,提供外部血糖测量的视觉警报。对所有连续的糖尿病住院患者进行糖尿病管理和毛细血管血糖评估。主要结果是记录了护理和医务人员对不良血糖发作(血糖> 15 mmol / l或<4 mmol / l)的反应。次要结果包括血糖测量。
研究显示对于不良血糖发作的反应,葡萄糖警报系统到位导致护理行为增加(与护理行动的比例:45%至73%; P <0.001),并且医疗行动增加(与医疗行动的比例:49%至67%; P = 0.011)。高血糖患者日(任何血糖值> 15 mmol/l:24%vs
16%; P = 0.012)和平均血糖(> 15
mmol / l)的患者日(7.4%vs 2.6%; P = 0.005)降低。低血糖发生率没有差异。
研究表明,使用新型葡萄糖警报系统改善了健康专业人员对不良血糖的反应并降低了医院环境中的高血糖症。
原始出处:
M. Kyi, P. R. Wraight, L. M. Rowan,et al.临床升级途径,墨尔本葡萄糖警报途径,以及(2)联网血糖仪,提供外部血糖测量的视觉警报。对所有连续的糖尿病住院患者进行糖尿病管理和毛细血管血糖评估。主要结果是记录了护理和医务人员对不良血糖发作(血糖> 15 mmol / l或<4 mmol / l)的反应。次要结果包括血糖测量。 研究显示对于不良血糖发作的反应,葡萄糖警报系统到位导致护理行为增加(与护理行动的比例:45%至73%; P <0.001),并且医疗行动增加(与医疗行动的比例:49%至67%; P = 0.011)。高血糖患者日(任何血糖值> 15 mmol/l:24%vs 16%; P = 0.012)和平均血糖(> 15 mmol / l)的患者日(7.4%vs 2.6%; P = 0.005)降低。低血糖发生率没有差异。 研究表明,使用新型葡萄糖警报系统改善了健康专业人员对不良血糖的反应并降低了医院环境中的高血糖症。 原始出处: M. Kyi, P. R. Wraight, L. M. Rowan,et al. Glucose alert system improves health professional responses to adverse glycaemia and reduces the number of hyperglycaemic episodes in non‐critical care inpatients 本文系梅斯医学(MedSci)原创编译整理,转载需授权!"> Glucose alert system improves health professional responses
to adverse glycaemia and reduces the number of hyperglycaemic episodes in non‐critical
care inpatients
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#DIA#
24
#专业人员#
29
#Diabetic#
27
#BET#
25
#高血糖#
36
#监护#
28
#Med#
23