老年套细胞淋巴瘤研究进展
2016-09-07 哈尔滨医科大学附属肿瘤医院 中国肿瘤
来源:中国肿瘤2016,25(9):715-720作者:余长艳,周雪萌,赵曙,张悦,张清媛作者单位:哈尔滨医科大学附属肿瘤医院套细胞淋巴瘤(MCL)是NHL的一种亚型,相对少见,占NHL的3%~10%。MCL患者以老年居多,中位发病年龄为65岁,男性多于女性,男∶女约2~3:1。迄今为止未发现与MCL发病明确相关的危险因素,伯氏包柔螺旋体(borrelia)可能是MCL发病的危险因素之一,但其
来源:中国肿瘤2016,25(9):715-720
作者:余长艳,周雪萌,赵曙,张悦,张清媛
作者单位:哈尔滨医科大学附属肿瘤医院
套细胞淋巴瘤(MCL)是NHL的一种亚型,相对少见,占NHL的3%~10%。MCL患者以老年居多,中位发病年龄为65岁,男性多于女性,男∶女约2~3:1。迄今为止未发现与MCL发病明确相关的危险因素,伯氏包柔螺旋体(borrelia)可能是MCL发病的危险因素之一,但其确切机制尚未明确。此外有研究发现某些MCL发病存在家族聚集的现象,提示MCL的发病可能存在遗传学因素。总之,MCL的发病机制较为复杂,其主要的致病机制包括细胞周期失控、DNA损伤修复途径异常以及核因子κB(NF-κB)通路的异常激活。多数患者确诊时已为晚期(Ⅲ期~Ⅳ期)。
MCL在疾病初期可表现为缓慢无痛性、进行性淋巴结肿大,疾病进展期表现为全身淋巴结肿大。近90%的MCL有结外侵犯:肝脏、脾、骨髓、胃肠道及中枢神经系统浸润,自发性脾破裂是其少见的并发症;25%~50%的病例可见外周血淋巴细胞增多;较少见的结外病变部位还包括皮肤、肺、乳腺、软组织、唾液腺及眼眶;50%的病例可有贫血、乳酸脱氢酶(LDH)升高和β2-微球蛋白升高;25%~50%的患者有B症状。MCL因其具备独特的形态学、免疫学及细胞遗传学特征而受到关注。MCL预后较差,中位总生存时间(OS)仅4~5年。近年来得益于免疫化疗、干细胞移植以及挽救治疗的进展,使MCL的疗效有了显著提高。现就MCL的最新研究进展,特别是老年患者的治疗进展作一综述。
一、病理生理
MCL起源于淋巴结淋巴组织滤泡层未受抗原刺激的周围性B淋巴细胞。经典MCL细胞缺乏类似于中心母细胞的肿瘤性转化细胞、副免疫母细胞和增殖活跃的生发中心。肿瘤细胞表达细胞膜IgM或IgD,有免疫球蛋白轻链限制性表达(λ轻链限制多见),表达CD5、FMC-7、CD43、SIgM(+),SIgD(+),CD19(+)、CD20(+)、CD22(+)、CD79a(+)、CD74(+)、Bcl-2,95%以上的MCL有t(11;14)(q13;q32)染色体易位,导致细胞周期D1(CCND1)蛋白过度表达,少数MCL中CCND1为阴性,但常有CyclinD2/3的过度表达,然而单纯t(11;14)移位伴CyclinD1过表达并不能发展为淋巴瘤,还需要与其他继发的细胞遗传学异常一起作用。继发的细胞遗传学改变包括染色体3q+、7p+、8q+、12q+、18q+等增加和1p-、6q-、8p-、9p-、9q、11q、13q、17p等缺失,这些染色体异常可导致相关基因的突变,或异常表达,或信号转导通路改变。MCL不表达CD10、Bcl-6、CD23,多数MCL表达SOX11。SOX11转录因子在CyclinD1过度表达的经典型MCL和无CyclinD1过度表达的MCL中均增加,阴性者则临床进程为惰性,生存期较长。除上述经典型外,MCL还有母细胞型、小细胞型、单核细胞样型和多形性母细胞型等其他类型。
二、MCL治疗
普遍认为MCL兼具惰性和侵袭性NHL两者最差的特征,因其常规化疗不能根治,且生长方式更具侵袭性。目前MCL仍无标准的治疗方案,近年来随着新药的不断出现,MCL患者的生存得到显著改善。
1、新诊断MCL的一般治疗原则
1.1 局限期MCL的治疗
约6%~8%的MCL确诊时为局限期(Ⅰ~Ⅱ期)。Leitch等统计了26例局限期MCL患者的临床特征及预后,发现在化疗基础上给予受累野放疗可显著提高局限期MCL的疗效。特别值得一提的是,在17例接受放疗的患者中,35.3%在治疗5年后依然无疾病进展。近期的另一项回顾性研究,总结了26例局限期MCL患者的疗效,得出了相同的结论。总反应率(ORR)及局部控制率均达95%,中位无进展生存期(PFS)和OS分别为3.2年和6.4年,系统复发在Ⅱ期患者中更为普遍。综上,对于局限期MCL患者,在化疗基础上(包括免疫治疗)联合受累野放疗是合适的选择。
1.2 年轻、骨髓移植候选者的治疗
对于年轻患者,目前认为大剂量化疗联合自体外周血干细胞移植(ASCT)可显著提高患者的缓解率,并得到满意的生存质量。研究显示,在化疗中加入利妥昔单抗可显著提高MCL的疗效,延长患者的生存。MCL治疗的另一个重要进展是最近的几项研究证实含大剂量阿糖胞苷的化疗方案可显著提高疗效。一项SWOG0213研究结果显示,R-hyper-CVAD/MTX-Ara-C方案的完全缓解/未证实的完全缓解(CR/CRu)约55%,3年PFS和OS分别为66%和81%,中位随访4.8年的中位PFS和OS分别为4.8年和6.5年,这一方案虽然有更高的CR和更长的生存期,但化疗造成的血液系统不良事件发生率显著增加,尤其在年龄>65岁的老年患者中表现更为明显,因此不宜作为老年MCL的标准治疗方案。
此外,MCL治疗领域的最大进展在于发现ASCT可显著延长MCL的疗效。一项Ⅱ期研究表明,与标准蒽环类方案比较,ASCT前采用阿糖胞苷和利妥昔单抗方案诱导化疗者的5年无复发生存率(EFS)和OS分别达64%和75%,ASCT前采用高剂量阿糖胞苷化疗将CR率从69%上升到96%,延长了MCL患者长期无病生存率。
综上,对于适宜行ASCT的年轻MCL患者,含大剂量阿糖胞苷的化疗方案联合利妥昔单抗治疗是目前的标准一线方案。
2、老年MCL患者的治疗选择
2.1 老年患者的一线治疗
通常临床上将年龄>65岁的患者定义为老年患者,老年淋巴瘤患者的预后较差,与治疗时给药剂量不足、药物代谢在体内发生改变、老年人常合并其他疾病和脏器功能异常等因素有关。如前所述,MCL的中位发病年龄为65岁,因此充分考虑老年人群的自身特点,设计个体化的治疗方案,改善老年MCL的预后是亟待解决的问题。对于Ⅰ/Ⅱ期低危老年MCL患者,考虑到治疗相关并发症,可仅予以观察。
单中心研究显示延迟治疗并不影响低危患者的OS,尤其对肿瘤负荷低、Ki67低表达、无症状的老年患者。对于需要治疗的患者,R-CHOP方案仍是目前的标准方案,ORR可达85%左右,CR为30%~40%,中位复发时间为2~3年。氟达拉滨(fludarabine)是一种抗代谢性细胞毒化疗药物,最近欧洲MCL工作组的一项随机对照研究探讨了含氟达拉滨的化疗方案在MCL一线治疗中的疗效。560例超过60岁(中位年龄70岁)的老年MCL患者随机接受8个周期R-CHOP方案或6个周期R-FC方案化疗,有效者随机接受α干扰素或利妥昔单抗维持治疗直至疾病进展。研究结果显示新的诱导治疗未改善预后,ORR方面R-CHOP组为86%,R-FC组为78%;CR率分别为34%和40%,亦无统计学差异;总生存方面R-CHOP组优于R-FC组(4年OS:62%vs40%)。在不良反应方面R-FC组更明显,尤其是血液学毒性和感染发生率显著高于R-CHOP组。在维持治疗方面,利妥昔单抗显示出更大优势,4年无进展生存时间利妥昔单抗维持治疗组为58%,显著高于α干扰素治疗组(28%),RCHOP诱导治疗后续利妥昔单抗维持治疗的4年OS达85%。
此外,一些研究还探讨了更强烈的化疗方案在老年MCL一线治疗中的价值。一项Ⅱ期前瞻性研究中,97例老年MCL患者接受R-HyperCVAD/MTX-Ara-C方案化疗而无后续大剂量化疗(HDT)及ASCT治疗。随访10年的结果显示中位TTF为4.6年,中位OS未达到。虽然疗效显著,但不良反应特别是黏膜炎及血液学毒性亦非常显著,化疗相关死亡率达8%。因此,由于显著的毒性反应,不推荐R-HyperCVAD/MTX-Ara-C用于老年MCL患者。苯达莫司汀(bendamustine)是一种新的氮芥类烷化剂。一项Ⅲ期研究中,对比了BR与R-CHOP一线治疗老年惰性及MCL的疗效。中位随访45个月的结果显示BR组的PFS显著延长(69.5个月vs31.2个月,P<0.0001)。BRIGHT研究的结果也显示BR在疗效上不劣于R-CVP和R-CHOP方案,且BR组患者化疗后的一般状态评分更高。基于上述研究的数据,8周期R-CHOP方案后续利妥昔单抗维持治疗仍是目前老年MCL患者标准治疗。BR方案也是老年MCL的理想治疗选择,尤其对于那些无法耐受阿霉素导致心脏毒性的患者。
2.2 虚弱老年患者的一线治疗
蒽环类药物是R-CHOP方案中许多不良反应的主要原因,如恶心、呕吐及中性粒细胞减少,蒽环类药物还有增加心脏毒性的风险。因此,对于较虚弱的老年患者,用R-CVP替代R-CHOP方案也是可行的。此外,对于较虚弱的老年患者,利妥昔单抗联合苯丁酸氮芥口服也是一种可接受的治疗选择,多数患者能够耐受该方案治疗。与滤泡淋巴瘤相比,利妥昔单抗单药治疗MCL的效果有限,总有效率约27%,无事件生存时间仅为6个月。
2.3 复发/进展期老年MCL的治疗
一线方案虽然显著提高了MCL的疗效,但几乎所有患者最终都会出现疾病复发或进展。对于复发/进展期MCL,目前尚无标准治疗方案,常用的治疗方案如Table 1所示。如前所述,BR方案是治疗MCL的有效方案,并可用于复发的病例,在该方案中加入米托蒽醌也是一种选择,三者联合的ORR为89%,其中CR率达35%,提示苯达莫司汀联合化疗可作为复发/难治MCL的治疗选择。

虽然在一线治疗中,R-FC与R-CHOP比较未显示出生存优势,甚至增加了毒性,然而氟达拉滨仍然是治疗MCL的有效药物,关键是如何选择合适的治疗人群。此外,有研究表明在R-FC基础上加入米托蒽醌(R-FCM)后ORR可达58%~79%,提示R-FCM对MCL有效。但是,考虑到蒽环类药物的心脏累积毒性,R-FCM方案可能不适合用于既往接受过RCHOP方案治疗的患者。
多数老年患者在一线治疗中未接受大剂量阿糖胞苷化疗,近期一项Ⅱ期试验研究了R-BAC在老年患者中的疗效。研究发现R-BAC方案虽然有效,但骨髓抑制反应较重。克拉屈滨(Cladribine)为嘌呤核苷酸类似物,在治疗恶性惰性淋巴瘤方面显示出较好的疗效。Robak等采用RC/RCC方案(利妥昔单抗、克拉屈滨、环磷酰胺)治疗B细胞淋巴瘤,其中9例MCL患者的ORR达67%,CR为11%。在另一项小型临床研究中,克拉屈滨单药治疗复发MCL(n=25),ORR和中位PFS分别为46%和5个月,并且不良反应相对较低。
硼替佐米(bortezomib)为蛋白酶体抑制剂,通过选择性与蛋白酶体活性位点的苏丝氨酸结合,可逆性抑制蛋白酶体26S亚单位的活性,显著减少NF-κB的抑制因子I-κB的降解,进而抑制细胞增殖相关基因的表达,最终导致细胞凋亡。硼替佐米单药治疗MCL的有效率为47%,该药的主要副作用是神经毒性,包括感觉神经病变及神经性疼痛。目前该药在美国已被批准用于治疗复发/进展期MCL,
此外有研究正在探讨硼替佐米联合阿糖胞苷的疗效,而降低剂量的联合治疗似乎也可适用于老年患者。哺乳动物雷帕霉素靶蛋白(mTOR)为丝苏氨酸激酶,在PI3K-Akt-mTOR通路中位于Akt下游,在调控蛋白合成、血管新生和细胞周期等细胞基本生命活动过程中发挥重要作用。
替西罗莫司(temsirolimus)为mTOR抑制剂,能引起细胞周期阻滞、抑制肿瘤细胞生长;在复发/难治性MCL中,单药替西罗莫司的有效率约38%,CR率为3%,平均有效时间6个月。替西罗莫司主要不良反应包括血小板减少、腹泻和乏力等,该药在欧洲已被批准用于治疗复发MCL。
3、MCL治疗的最新进展
雷利度胺(Lenalidomide)和沙利度胺(Thalidomide)是一种免疫调节药物,它们能干扰肿瘤血管生成及其微环境,增强自然杀伤细胞(NK)对肿瘤的杀伤能力,是治疗多发性骨髓瘤的药物,在MCL治疗中也取得了可喜的成果。应用雷利度胺联合剂妥昔单抗治疗38例MCL患者,ORR为92%,CR为64%,3年OS为97%,这些指标都明显优于传统治疗方案,提示沙利度胺联合利妥昔单抗对MCL有明显治疗效果。
此外,沙利度胺是一种副作用较小的口服制剂,沙利度胺联合利妥昔单抗治疗16例难治复发的MCL患者,ORR为81%,CR率为31%,3年DFS为20.4个月,3年OS为75%,提示其在维持治疗中非常有价值。目前,有研究正在探讨该类药物维持治疗中的价值,结果值得期待。
Bruton’s酪氨酸激酶(BTK)是细胞生理活动中的一个重要蛋白,参与介导B细胞的迁移、趋化及粘附等生物学活性。依鲁替尼(Ibrutinib)是小分子BTK抑制剂,能够与BTK活性中心的半胱氨酸残基共价结合,从而抑制其活性。临床前研究证明,依鲁替尼能够抑制恶性B细胞的增殖和生存。一项多中心Ⅱ期临床试验评价了依鲁替尼治疗复发/难治性MCL的疗效,111例可评价病例,中位随访15.5个月,总ORR为68%,CR为21%,中位应答时间17.5个月,中位PFS为13.9个月,主要不良反应包括血液学毒性、肺炎、腹泻和疲乏等。目前,依鲁替尼已被FDA批准用于治疗MCL。
PI3K/AKT/mTOR信号传导途径是细胞内非常重要的信号转导途径,在细胞生长、存活、增殖、凋亡、血管生成、自噬过程中发挥重要作用,针对该途径的新型靶向药物是近年来肿瘤治疗领域的研究点。GC1101(idelalisib)、wortmannin、LY294002等为PI3K抑制剂,edelfosine、perifosinr及PX2316为AKT抑制剂,Pimasertib为MEK的抑制剂,这些药物在MCL治疗中的价值正在探讨中。
三、预后
MCL具有独特的病理学和临床表现,兼具惰性和侵袭性NHL两者最差的特征。惰性MCL典型临床表现通常是白细胞增多和脾肿大,无淋巴结肿大。除罕见的惰性MCL外,大多数患者需要治疗以减少症状、防止疾病进展。有淋巴母细胞样变的MCL患者,疾病进展迅速,且对化疗不敏感,预后较差。
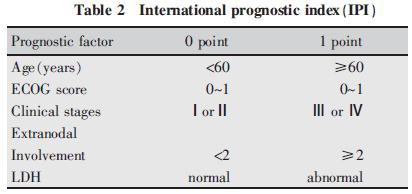
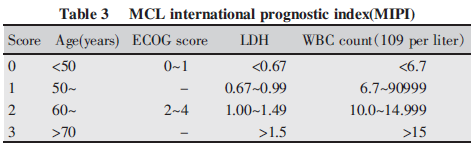
国际预后指数(IPI)(Table 2)评分对MCL预后的预测价值有限。德国/欧洲学者在2008年提出的套细胞淋巴瘤国际预后评分(MIPI)有更大的临床意义,该评分有4个独立预测因子:年龄、体能状态、乳酸脱氢酶和白细胞计数。据此将MCL分为三组(Table 3):低危组,0~3分,占44%,5年OS为60%;中危组,4~5分,占35%,中位OS为51个月;高危组,6~11分,占21%,中位OS为29个月。此外,Ki-67作为重要的生物标记,与预后亦密切相关。
四、小结
MCL是一种相对少见的NHL类型,半数以上患者为65岁以上的老年人,不能耐受大剂量化疗及ASCT,预后相对较差。虽然近年来多种新药的引入显著提高了MCL患者的疗效,患者的生存和预后都获得一定改善,但是MCL最终仍会出现疾病进展,如何进一步理解MCL的异质性、寻找确切的靶点、进行新药的开发,是未来研究的重点。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#细胞淋巴瘤#
32
继续关注,学习
56
#研究进展#
31
谢谢分享!!!!!!!
58
继续关注!!!!!!
57
继续学习
50
继续关注
43