AIM:临床医生需警惕间期结直肠癌的种族/民族差异
2017-05-25 MedSci MedSci原创
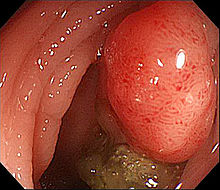
间期结直肠癌(Interval colorectal cancer,intervalCRC)也称为结肠镜后结直肠癌(post-colonoscopy colorectal cancer, PCCRC),定义为筛查或监测检查未发现,而在推荐的下一次检查日期之前发生的结直肠癌。在美国,间期CRC占所有CRC患者的3%-8%。但关于间期CRC的种族/民族数据却很少。因此,来自美国的研究人员进行了一项研究
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












高度警惕间期结直肠癌的差异。
71
学习并分享!!!
55
很好的文章,启示很多!
59
#结直肠#
36
#临床医生#
34
非常好的文章,学习了,很受益
54
谢谢分享,学习了
63
很好
26
学习谢谢分享
29
好好努力学习
27