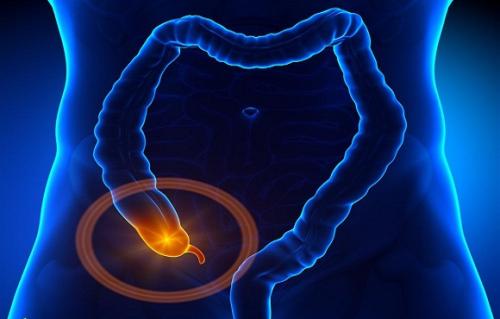
Radiology:FDG PET/MRI联合肝细胞特异性对比剂在直肠癌M分期的价值
2020-05-22 shaosai MedSci原创
PET/MRI在评价直肠癌远处转移(M分期)的价值与对比增强CT相比孰优孰劣尚不清楚。
背景
PET/MRI在评价直肠癌远处转移(M分期)的价值与对比增强CT相比孰优孰劣尚不清楚。
目的
本研究旨在比较氟18氟脱氧核糖(FDG)PET/MRI与胸腹部CT及直肠MRI在评价直肠癌临床M分期的价值差异。
材料与方法
本研究纳入了新诊的高级别中低位直肠癌的患者。患者均行FDG PET/MRI(包括肝脏和直肠MRI)、胸腹部CT检查(常规临床检查方案)。此后,以6个月临床随访或活检作为参考标准评价M分期的结果。比较两种方案的结果。并评估M分期的一致性。采用非参数检验进行统计学分析。
结果
本研究功能纳入了71例受试者。由于病变的不确定性共有22/71例患者(31%; 95% CI: 20.5%, 43.1%)通过常规临床检查方案不能明确其M分期。然而,在这些患者中,PET/MRI准确的识别了14例无转移(100%; 95% CI: 76.8%, 100%)及7/8例(88%; 95% CI: 47.4%, 99.7%)随访中发生转移的患者。PET/MRI在排除转移性病变较常规临床检查方案具有较高的特异性(98% [54/ 55例] vs 72% [40/55 例]; P < .001),并且不增加漏诊转移的患者(6% [1/16例] vs 6% [1/ 16例]; P > .99)。
结论
包含直肠和肝脏MRI的PET/MRI通过评价未知病变性质、转移有助于对新诊晚期直肠癌分期,其效果要由于对比增强CT检查,减少了额外的影像学检查。
原始出处:
Yoon JH, Lee JM, Chang W.et al. Initial M Staging of Rectal Cancer: FDG PET/MRI with a Hepatocyte-specific Contrast Agent versus Contrast-enhanced CT.
DOI:10.1148/radiol.2019190794
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#肝细胞#
33
#PET/MRI#
37
#特异性#
39
#细胞特异性#
43
#PE#
32
#PET#
30