Clin Gastroenterology H: 诊断显微结肠炎进行升结肠和降结肠的活检就够了
2020-08-09 MedSci原创 MedSci原创
病理表型为淋巴细胞性结肠炎和胶原性结肠炎通常会引起以慢性水样腹泻为主要症状的微观结肠炎(MC),但结肠镜检查并不能发现MC的宏观特征。
病理表型为淋巴细胞性结肠炎和胶原性结肠炎通常会引起以慢性水样腹泻为主要症状的微观结肠炎(MC),但结肠镜检查并不能发现MC的宏观特征。因此,内镜医师通常会收集多个随机的结肠活检样本最大可能进行活检检查,可能会取样过多,从而增加结肠镜检查时间。本项实验旨在试图确定怎样的活检顺序可以最大程度提高MC患者检出率。
研究人员采用回顾性研究方法,对2017年至2018年间无合并症的101例连续MC患者(52例胶原性结肠炎,42例淋巴性结肠炎)进行事后分析。在每个活检部位均计算出MC的诊断值。
研究结果显示:MC呈阳性的活检来自结肠每个部位的活检碎片的比例如下:盲肠,为90.0%;盲肠为90.0%;盲肠为90.0%。升结肠,96.9%; 肝弯曲,77.8%; 横结肠,95.7%; 脾弯曲,75.0%; 降结肠,85.0%; 乙状结肠,90.9%; 和直肠,占82.2%。对于标记为随机的活检,MC阳性率为95.7%。将结肠活检的上升和下降结果结合起来,就可以检测出100%的MC病例。
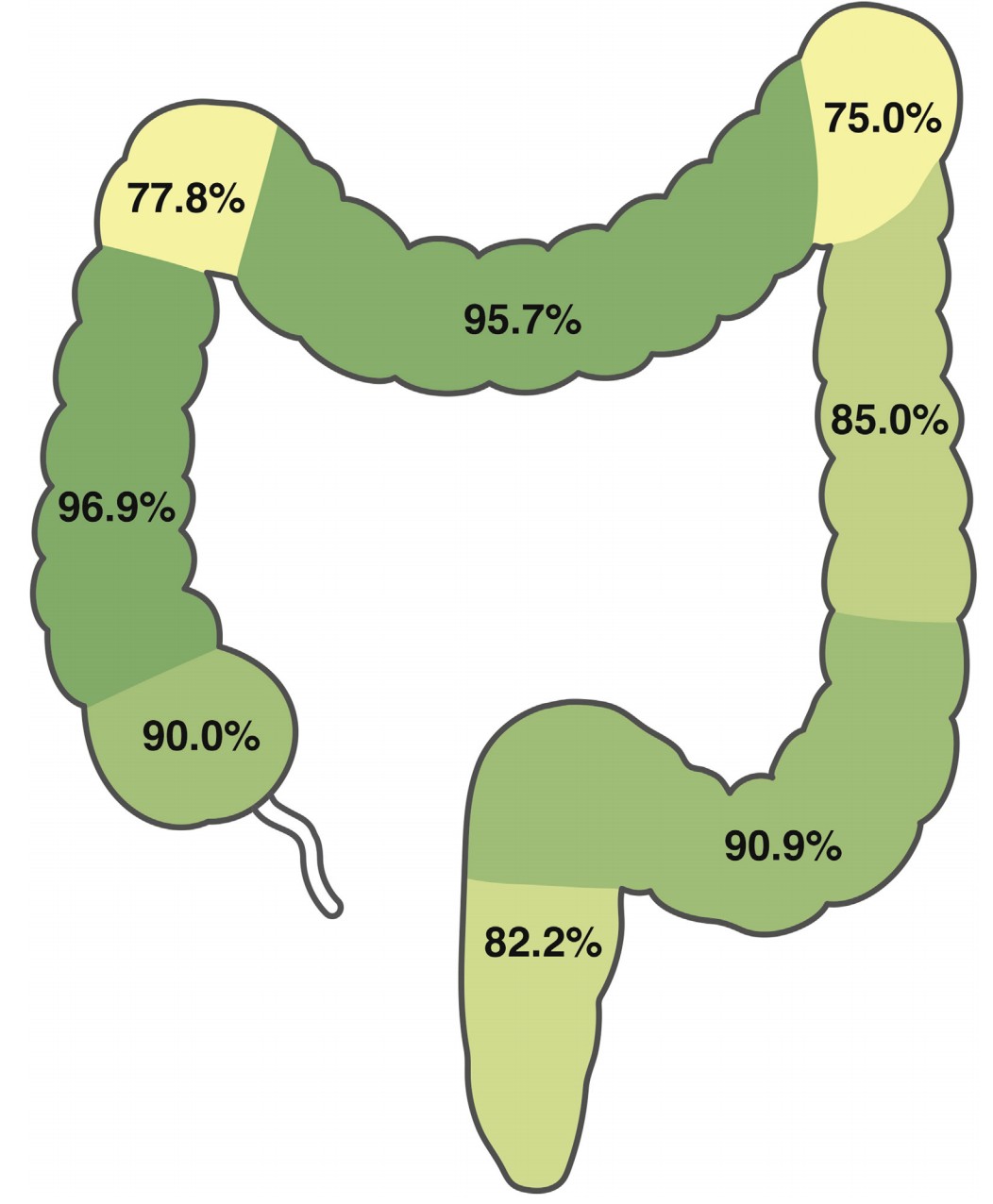
通过分析来自升结肠和降结肠的活组织检查可以确定地检测到MC,从升结肠和降结肠中进行两次活检就能够100%筛查出MC患者。
原始出处:
Boris Virine. Et al. Biopsies From Ascending and Descending Colon Are Sufficient for Diagnosis of Microscopic Colitis. Clin Gastroenterology H.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#AST#
29
#GAS#
33
#Gastroenterol#
32
厉害!
77
#活检#
30
#Gastroenterology#
24
#显微结肠炎#
34