NEJM:一例关于食管胃旁路的案例报道
2016-04-21 MedSci MedSci原创
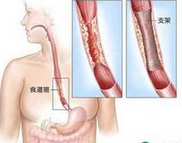
男性,60岁,以往进行过食管手术。 据了解,该患者在儿童时期曾因食道受到碱性烧伤,导致食管完全性狭窄。 在1962年(7岁),该患者接受了食管胃旁路手术(包括颈部食管结肠吻合术和腹内空肠结肠吻合术)。 体格检查发现,其胸部位置的近端食管胃旁路(结肠段)在腹部筋膜腹壁形成外突明显的疝。 吞水试验表明,该患者仍然具有正常的吞咽功能(请点击原始链接观看视频)。 会诊医师根据
男性,60岁,以往进行过食管手术。

据了解,该患者在儿童时期曾因食道受到碱性烧伤,导致食管完全性狭窄。
在1962年(7岁),该患者接受了食管胃旁路手术(包括颈部食管结肠吻合术和腹内空肠结肠吻合术)。
体格检查发现,其胸部位置的近端食管胃旁路(结肠段)在腹部筋膜腹壁形成外突明显的疝。
吞水试验表明,该患者仍然具有正常的吞咽功能(请点击原始链接观看视频)。
会诊医师根据该患者自身的情况,建议其进行疝修补术,但该患者出于对手术风险过大的担心,最终拒绝了手术治疗。
在过去,食管胃旁路术通常会被选择作为类似本案例中的病人进行治疗,因为这样病人可以避免发现其他的手术并发症和胸廓切开或胸骨后隧道术的麻醉。
目前,在临床上已经很少有直肠代食管,以及通过皮下定位食管替代术了。
原始出处:
Goran Marjanovic, M.D., and Jens Hoeppner, M.D. Esophagogastric Bypass in Motion
N Engl J Med 2016; 374:e20April 21, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











不错哦,会学到很多
53
#胃旁路#
42
可怕的图片
73
#食管#
29