Cell Death Dis:类固醇激素合成介导肾上腺皮质细胞铁死亡
2020-04-03 MedSci原创 MedSci原创
目前对于肾上腺皮质细胞死亡反应的了解甚少,但其极具临床意义。在Addison病中,肾上腺皮质细胞的破坏导致肾上腺类固醇匮乏,如果不加以治疗则可能会致命。
铁死亡是一种铁依赖性的细胞死亡形式,与脂质过氧化反应增强相关。
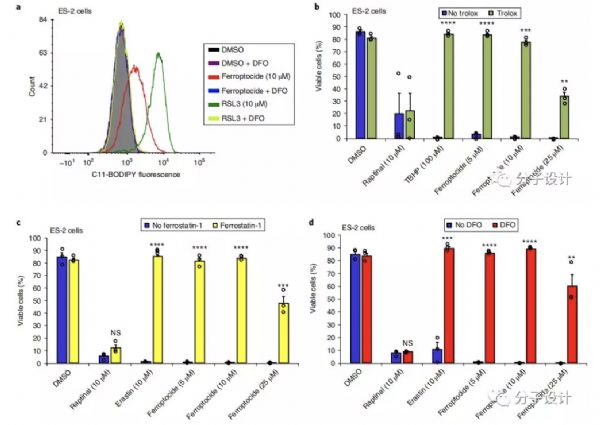
研究人员发现GPX4(谷胱甘肽过氧化物酶4)和ACSL4(长链脂肪酸CoA连接酶4)这两个引起铁死亡的关键基因在肾上腺皮质中具有高表达水平。采用MALDI质谱成像分析正常及肿瘤肾上腺皮质组织,研究人员检测到高水平的花生四烯酸及肾上腺酸,这两种长链多不饱和脂肪酸在铁死亡的治疗过程中发生了过氧化反应。研究人员发现在三种肾上腺皮质细胞系(H295R,CU-ACC1及CU-ACC-2)中,RSL3对GPX4抑制作用具有高度敏感性,EC50值分别是5.7×10-8、8.1×10-7 和2.1×10-8;而在所有非类固醇生成细胞中该敏感性均显著降低。
通过RSL3完全阻断GPX4的活性可导致铁死亡的发生,在肾上腺皮质细胞中使用酮康唑抑制类固醇的生成可以完全逆转该作用,但使用美替拉酮阻断皮质醇合成的最终步骤不能逆转该反应。尽管会诱导ACC细胞脂质过氧化反应,米托坦是批准用于ACC治疗中唯一不会引起铁死亡的药物。
总而言之,该研究首次证明了肾上腺皮质细胞对铁死亡反应的高敏感性是通过活性类固醇合成途径介导的。在ACC治疗中,密妥坦不会诱导这种形式的细胞死亡。
原始出处:
Weigand et al. Active steroid hormone synthesis renders adrenocortical cells highly susceptible to type II ferroptosis induction. Cell Death and Disease (2020) 11:192
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#肾上腺#
36
#CEL#
23
#肾上腺皮质细胞#
34
#Cell#
22
#类固醇激素#
25
#Dis#
22
#类固醇#
27
#Death#
25