Blood:以PET-CT分层可提高滤泡性淋巴瘤患者的放射治疗效果
2018-11-17 MedSci MedSci原创
中心点:经PET-CT进行分层后,I期和局限性II期滤泡性淋巴瘤放射治疗的预后要优于既往试验。三分之二以上的患者5年内一直保持缓解状态,而且大多数复发发生在边缘部位。摘要:放射治疗(RT)对局限性滤泡性淋巴瘤(FL)的疗效较好,既往表明FL患者的10年无进展存活率达40-50%。随着18F-FDG PET-CT的出现,其效果优于CT,现研究人员对以PET-CT分期的患者的预后进行评估,以明确更为精
经PET-CT进行分层后,I期和局限性II期滤泡性淋巴瘤放射治疗的预后要优于既往试验。
三分之二以上的患者5年内一直保持缓解状态,而且大多数复发发生在边缘部位。
摘要:
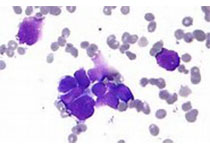
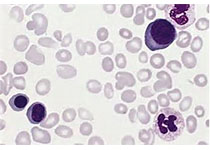
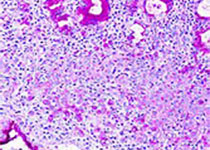
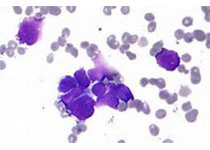
放射治疗(RT)对局限性滤泡性淋巴瘤(FL)的疗效较好,既往表明FL患者的10年无进展存活率达40-50%。随着18F-FDG PET-CT的出现,其效果优于CT,现研究人员对以PET-CT分期的患者的预后进行评估,以明确更为精确的分期是否可提高患者的预后。
研究人员开展一多中心的回顾性研究,招募既往未治疗过的、以PET-CT分期的、仅采用放射治疗(剂量≥24Gy)的年满18岁的I-II期(1-3A)FL患者,且要求随访满3个月。结点为无进展存活率(FFP)、局部控制和总体存活率(OS)。
招募到于2000年-2017年在16个国家治疗的512位患者。中位年龄58UI(20-90)。410位患者(80.1%)为I期。中位放疗剂量为30Gy(24-52)。中位随访52个月(3.2-174.6)。五年FFP和OS分别是68.9%和95.7%。I期和II期患者的五年FFP分别为74.1%和49.1%。
8位患者复发(1.6%)。4位患者出现边缘复发(0.8%),局部控制率为97.6%。根据多变量分析,II期(HR 2.11,95% CI 1.44-3.10)和BCL2表达(HR 1.62,95% CI 1.07-2.47)与FFP不良关系密切。以PET-CT分期的患者放射治疗后的情况比早前试验中的好,特别是对于I期患者,提示放射治疗对于真正局限性FL的治疗潜能一直被低估了。
Jessica L. Brady,et al.Definitive radiotherapy for localized follicular lymphoma staged by 18F-FDG PET-CT: a collaborative study by ILROG.Blood 2018 :blood-2018-04-843540; doi: https://doi.org/10.1182/blood-2018-04-843540
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#治疗效果#
0
#PE#
31
#滤泡性淋巴瘤#
40
#PET#
40
#PET-CT#
42
谢谢梅斯提供这么好的信息,学到很多
48
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
46
了解一下,谢谢分享!
61