J Clin Oncol:外周血cfDNA中的肿瘤分数可以预测转移性三阴性乳腺癌的预后
2018-01-06 肿瘤资讯编辑部 肿瘤资讯
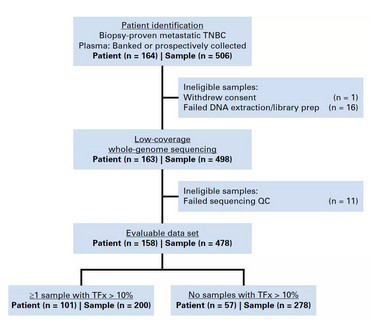
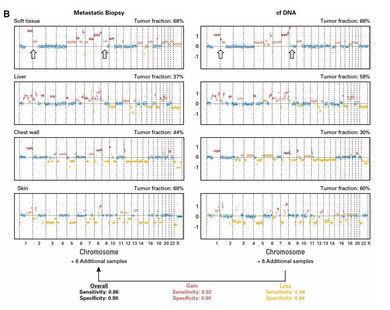
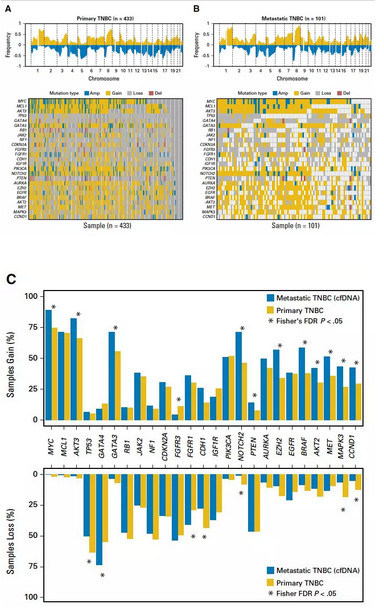
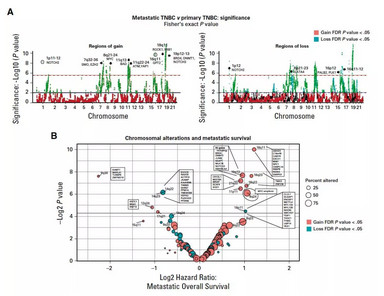
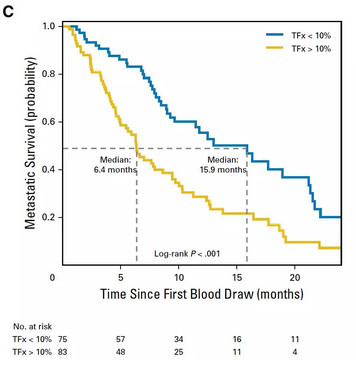
三阴性乳腺癌只占乳腺癌总体的15%,但却导致了25%以上但乳腺癌相关死亡。过去20年,TNBC患者的总生存没有显着变化。目前,化疗是TNBC主要的治疗手段。对TNBC进行基因组学分析,可能可以发现潜在的生物标志物,指导治疗或预测预后。近日,发表在《JCO》杂志上的研究,采用创新性的方法对转移性三阴性乳腺癌中外周血标本进行检测,发现了重要的预后指标。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#cfDNA#
58
#Oncol#
48
#阴性乳腺癌#
46
#转移性三阴性乳腺癌#
47
#转移性#
48
#三阴性#
49
#外周血#
35
三阴性乳腺癌只占乳腺癌总体的15%.但却导致了25%以上但乳腺癌相关死亡
79
谢谢分享.学习了
67