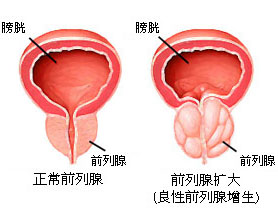
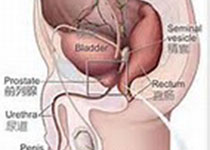
Phytother Res:百里醌对睾丸素诱导的良性前列腺增生具有抑制作用
2017-10-04 AlexYang MedSci原创
最近,有研究人员阐释了在大鼠中,百里醌(TQ)对试验条件下诱导的良性前列腺增生(BPH)的发展具有可能的保护性作用。在试验中,18只成年雄性大鼠分为3个小组;阴性对照组(n=6)接受介质注射,另外两个组接受皮下睾丸素注射(3mg/kg)。再将接受睾丸素注射的大鼠随机分成BPH不处理组(n=6)和BPH+TQ处理组(n=6,5mg/kg口服14天)。研究人员还分析了组织学变化和转变生长因子-β1(T
最近,有研究人员阐释了在大鼠中,百里醌(TQ)对试验条件下诱导的良性前列腺增生(BPH)的发展具有可能的保护性作用。在试验中,18只成年雄性大鼠分为3个小组;阴性对照组(n=6)接受介质注射,另外两个组接受皮下睾丸素注射(3mg/kg)。再将接受睾丸素注射的大鼠随机分成BPH不处理组(n=6)和BPH+TQ处理组(n=6,5mg/kg口服14天)。研究人员还分析了组织学变化和转变生长因子-β1(TGF-β1)以及血管内皮生长因子A(VEGF-A)的mRNA水平。另外,研究人员还定量了二氢睾酮和白介素-6(IL-6)血清水平。研究表明,在BPH大鼠未处理组,前列腺重/体重比值、前列腺表皮厚度、血清IL-6和二氢睾酮水平、TGF-β1和VEGF-A的前列腺表达水平均显著增加。在BPH大鼠中的前列腺组织检查表明了基质区域和腺上皮增殖水平提高,并且具有丰富的管腔内的乳头状褶皱。然而,研究人员在BPH+TQ处理大鼠中与未处理BPH大鼠比较,观察到了前列腺重/体重比值、前列腺表皮厚度、血清IL-6和二氢睾酮水平、TGF-β1和VEGF-A的前列腺表达水平的减少。最后,研究人员指出,这些结果支持了T
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#抑制作用#
44
学习
415
#睾丸#
44
#睾丸素#
27
#良性前列腺增生#
48
谢谢分享.学习了
48
学习了.涨知识
47
不错的.学习了.谢谢分享!
49