Int J Mol Sci:特异性诱导多能干细胞在CFC患者中的成骨作用
2017-12-06 MedSci MedSci原创
心面皮肤(CFC)综合征是由细胞外信号调节激酶(ERK)通路突变引起的罕见遗传疾病。然而,关于ERK信号异常与大多数CFC综合征患者中表现出的骨发育缺陷之间的关联知之甚少。在这项研究中,从CFC综合征患者的真皮成纤维细胞中诱导性多能干细胞(iPSC)。将CFC-iPSCs分化为间充质干细胞(CFC-MSC),并在体外进一步诱导出成骨细胞。通过碱性磷酸酶活性测定,矿化测定,定量实时聚合酶链式反应(q
心面皮肤(CFC)综合征是由细胞外信号调节激酶(ERK)通路突变引起的罕见遗传疾病。然而,关于ERK信号异常与大多数CFC综合征患者中表现出的骨发育缺陷之间的关联知之甚少。
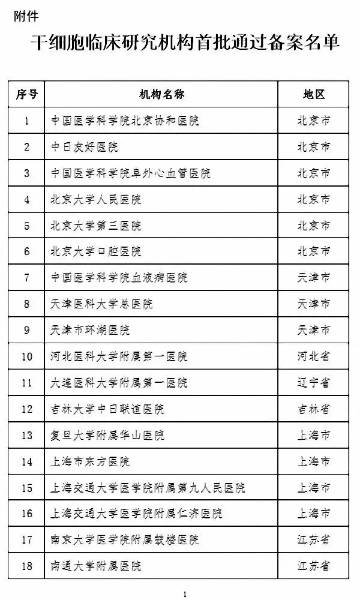
在这项研究中,从CFC综合征患者的真皮成纤维细胞中诱导性多能干细胞(iPSC)。将CFC-iPSCs分化为间充质干细胞(CFC-MSC),并在体外进一步诱导出成骨细胞。通过碱性磷酸酶活性测定,矿化测定,定量实时聚合酶链式反应(qRT-PCR)和western印迹显示CFC-MSCs的成骨缺陷。
结果显示,与野生型(WT)-MSCs相比,CFC-MSCs的成骨能力减弱。CFC-MSC在诱导成骨过程中,除了激活ERK通路,还发现p-SMAD2表达的升高和p-SMAD1表达的降低。通过抑制ERK和SMAD2信号传导或激活SMAD1通路可挽救CFC-MSC的成骨缺陷。重要的是,ERK和SMAD2信号传导的激活或SMAD1信号传导的抑制重演了WT-MSC中的成骨受损。
综上所述,该研究结果表明,SMAD2和SMAD1以及ERK通路是导致CFC综合征早期骨发育缺陷的原因,为了解该疾病的病理机制和治疗靶点提供了一个新的见解。
结果显示:
Choi JY, Han KM, et al., Impaired Osteogenesis of Disease-Specific Induced Pluripotent Stem Cells Derived from a CFC Syndrome Patient. Int J Mol Sci. 2017 Dec 1;18(12). pii: E2591. doi: 10.3390/ijms18122591.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#诱导多能干细胞#
36
#特异性#
32
#成骨#
27
谢谢分享谢谢分享!
61
间质性干细胞无所不能
49