Clin Trans Gastro:水通道蛋白在腹泻肠易激综合征结肠黏膜活检中的表达分析
2019-05-20 不详 MedSci原创
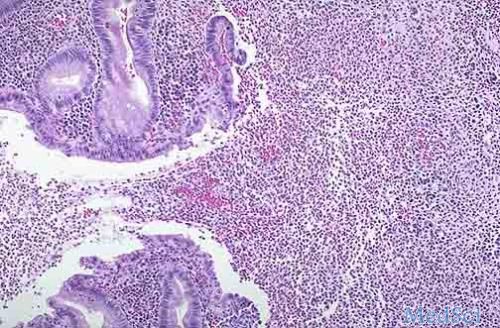
我们已知,水通道蛋白(AQP)通道参与调节结肠体液稳态,并且有文献报道,在人结肠上皮细胞中检测到几个AQP通道。在先前的研究中,喂食1%胆酸钠的大鼠其AQP3,7和8水平明显增加,表明AQP参与胆汁酸腹泻(BAD)。因此,本项研究的目的是比较肠易激综合征-腹泻(IBS-D)患者的直肠乙状结肠粘膜(RSM)活检中的AQP表达(分为正常或高粪便BA排泄的患者)和IBS-便秘患者(IBS-C) )与健康
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#GAS#
26
#TRA#
31
#表达分析#
38
#AST#
31
#活检#
20
#综合征#
26
#黏膜#
32