NEJM:皮肤白喉-病例报道
2018-03-29 xing.T MedSci原创
皮肤白喉早期表现可出现边界清楚的溃疡愈合。该病人进行白喉检测后,服用的抗生素改为克拉霉素。追踪接触者,并给家庭接触者进行药物预防。
患者为一名5岁完全接种疫苗的女孩,因双腿瘙痒性皮损而到急诊就诊。
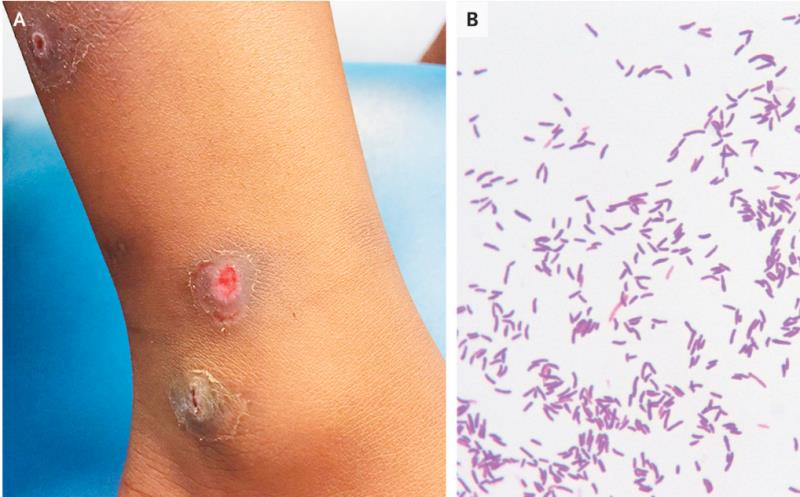
她最近刚从塞拉利昂旅行回来。她到那里3周后出现上述病灶,并且病灶有所增大,并且出现溃疡。在就诊过程中,她不发热,左小腿内侧区出现了溃疡和出血(如图A所示)。C反应蛋白水平轻度升高,白细胞计数正常。开始口服氟氯西林进行经验性治疗,并且进行皮肤拭子培养,其中金黄色葡萄球菌、A组链球菌和白喉棒状杆菌阳性。
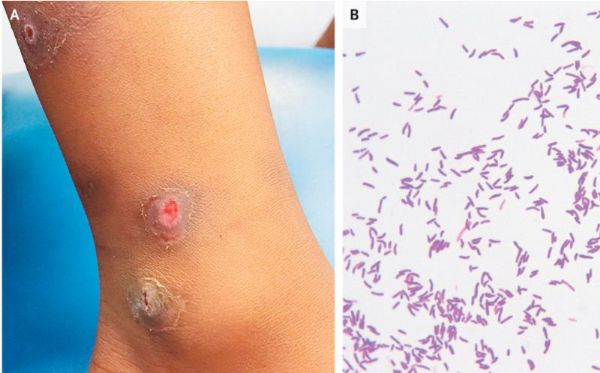
Gram染色显示革兰阳性杆菌主要以棒状杆菌为主(如图B所示)。免疫扩散试验(Elek’s试验)阳性,表明这是白喉毒素产生所致。皮肤白喉早期表现可出现边界清楚的溃疡愈合。该病人进行白喉检测后,服用的抗生素改为克拉霉素。追踪接触者,并给家庭接触者进行药物预防。
该患者在采用克拉霉素进行抗生素治疗1周后,皮损完全愈合。
原始出处:
Isabel E. Wilson,et al. Cutaneous Diphtheria.N Engl J Med 2018. http://www.nejm.org/doi/full/10.1056/NEJMicm1701825
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






学习学习学习
51
#白喉#
29
学习学习学习
46
好知识.值得学习
55
了解了解.学习学习
5