脑动静脉畸形的立体定向放射外科治疗了解一下?
2018-08-11 陈豪 陈如东 神经精神界
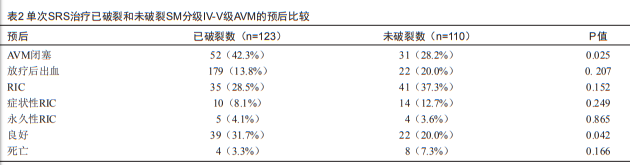
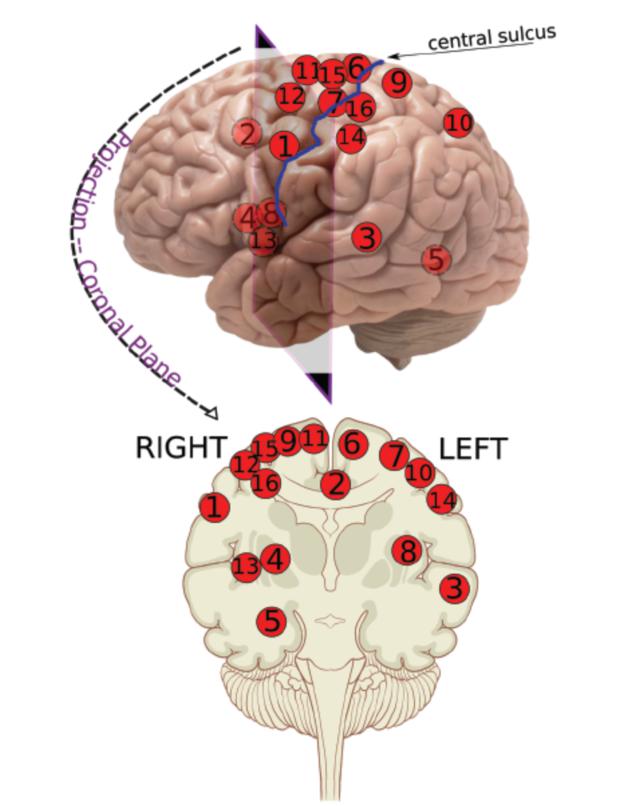
有研究显示其用于预测立体定向放射外科(stereotactic radiosurgery,SRS)治疗小AVM的预后也是可靠的;SM分级IV-V级AVM因其体积大、血管构筑复杂、部位险要等特点,难以成功治疗;SRS已广泛用于治疗手术切除困难的小AVM,但其治疗SM分级IV-V级AVM的有效性目前尚无共识。针对上述问题,Jason P. Sheehan等人进行了一项多中心、回顾性队列研究,该研究

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#动静脉畸形#
37
#定向#
25
#立体定向#
36
#静脉#
28
#畸形#
28
学习
61
学习
63