Nat Commun:这种胆固醇代谢产物“劫持”免疫细胞,让癌症扩散
2017-10-17 佚名 生物探索
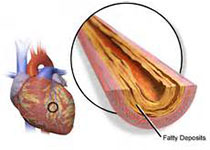
美国伊利诺伊大学的一项新研究发现,胆固醇的代谢产物——27羟基胆甾醇(27HC)作用于特定的免疫细胞,劫持免疫系统以促进癌症扩散,或是癌症转移的“罪魁祸首”。开发出抑制27HC的小分子药物,有望降低高胆固醇的癌症患者体内肿瘤细胞的扩散。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#癌症扩散#
51
#COMMUN#
46
#Nat#
35
#代谢产物#
39
学习啦!谢谢分享!
86