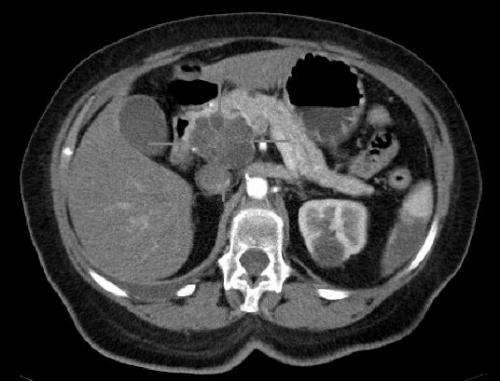
Sci Rep:靶向PAK4化合物有望用于胰腺癌治疗
2017-02-19 MedSci MedSci原创
一项新的研究证实了称为PAK4的蛋白质在胰腺癌细胞的运动和生长中的作用,可以帮助研究人员找到解决这种疾病的新方法。这项工作由国家慈善胰腺癌研究基金资助,发现了新的证据表明,PAK4使癌细胞生长和从胰腺扩散到身体的其他部位,在转移的过程中发挥关键作用。来自伦敦国王学院的研究人员也发现了PAK4与一种被称为磷酸肌醇3-激酶途径(PI3K)的癌症途径之间的密切关系的证据。PI3K负责调节癌细胞的生长和存
 胰腺癌细胞中的作用" style="border: 0px; max-width: 100%; display: block; margin: 10px auto;">
胰腺癌细胞中的作用" style="border: 0px; max-width: 100%; display: block; margin: 10px auto;">一项新的研究证实了称为PAK4的蛋白质在胰腺癌细胞的运动和生长中的作用,可以帮助研究人员找到解决这种疾病的新方法。
这项工作由国家慈善胰腺癌研究基金资助,发现了新的证据表明,PAK4使癌细胞生长和从胰腺扩散到身体的其他部位,在转移的过程中发挥关键作用。
来自伦敦国王学院的研究人员也发现了PAK4与一种被称为磷酸肌醇3-激酶途径(PI3K)的癌症途径之间的密切关系的证据。PI3K负责调节癌细胞的生长和存活,并且已经开发了靶向其的几种抑制剂。
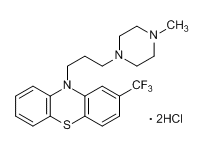
“我们已经看到PAK4和PI3K通路是联系在一起的,但是发现他们相互作用的证据是一个重要的进步,我们因此发现了解决这种疾病的有希望的新的抑制剂化合物”。
这项工作补充了对PAK4的现有研究,通过使用更好地模拟胰腺肿瘤的复杂模型系统,改进了现有知识。
该团队还研究了当PAK4从细胞中去除时发生了什么。
“这种技术使我们能够详细了解细胞的结构和发育,我们可以清楚地看到,如果从这些细胞中去除PAK4,它们就失去了侵袭的能力,”Wells博士解释说。
Wells博士补充说:“胰腺癌的一个重要问题是复发 - 即使对于可以手术的患者,也有非常高的复发率。如果我们可以开发抑制细胞移出胰腺的治疗方案,可以在手术后给予患者,并有助于预防该疾病的复发和传播。”
最终,该研究证实PAK4是新药物化合物的有希望的靶标,其中许多已经被研究人员鉴定用于测试。该团队还计划进一步研究,以了解更多关于胰腺癌细胞为什么依赖于PAK4。
原始出处:
King H, Thillai K, Whale A, Arumugam P, Eldaly H, Kocher HM, Wells CM. PAK4 interacts with p85 alpha: implications for pancreatic cancer cell migration. Sci Rep. 2017 Feb 16;7:42575. doi: 10.1038/srep42575.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#化合物#
32
文章真心不错耶
60
新的靶点,价值有待进一步研究…
54
好好努力
50
新发现,新治疗
47
希望能好好用在患者上
52
很有希望的治疗方法,谢谢分享
15
感谢分享!学习了!
25