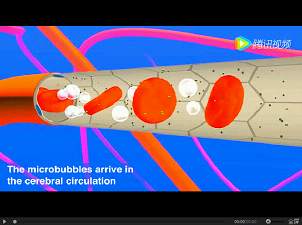
NAT MED:血脑屏障如何维持?
2017-03-14 wangzhe MedSci原创
已报道内皮G-蛋白偶联受体(GPCR)Gpr124是小鼠胚胎中正常前脑血管生成和BBB功能所必需的,但是该受体在成年动物中的作用是未知的。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
32
好好学习,好文章谢谢分享
49
#血脑屏障#
35
#Med#
33
学习了,谢谢了
61