Lancet:PEEP结合肺复张法不能预防开腹手术术后肺并发症
2014-10-08 leiqc 丁香园
目前关于术中全身麻醉期间采用机械通气中呼气末正压通气的作用仍不确定。 高于0 cm H2O 的压力水平或许能防止术后肺部并发症,但也可能导致术中循环抑制和过度膨胀造成的肺损伤。 因此,来自新西兰阿姆斯特丹大学重症监护医学与学术医学中心的Hemmes SN教授带领团队对开腹外科手术全身麻醉期间接受低换气量机械通气的有并发症风险患者采用高呼气末正压通气结合肺复张方法,探讨该方法是否可以防止术后肺部并
目前关于术中全身麻醉期间采用机械通气中呼气末正压通气的作用仍不确定。 高于0 cm H2O 的压力水平或许能防止术后肺部并发症,但也可能导致术中循环抑制和过度膨胀造成的肺损伤。
因此,来自新西兰阿姆斯特丹大学重症监护医学与学术医学中心的Hemmes SN教授带领团队对开腹外科手术全身麻醉期间接受低换气量机械通气的有并发症风险患者采用高呼气末正压通气结合肺复张方法,探讨该方法是否可以防止术后肺部并发症的发生。
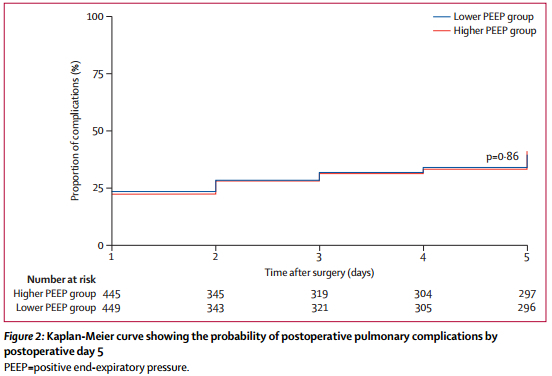
该研究是一项涉及欧洲、北美和南美30个中心的随机对照研究,共有900例全身麻醉和在 8 mL/kg 换气量通气条件下接受开腹手术且有术后肺部并发症风险的患者。研究者将患者随机分配至高呼气末正压 (12cm H2O) 结合肺复张组(高 PEEP 组)或低呼气末正压 (≤2 cm H2O) 不结合肺复张组(低 PEEP 组)。
研究者使用集中式计算机随机分配系统。患者和转归评估者均对干预措施不知情。主要观察指标是术后第 5 天的术后肺部并发症。采用意向治疗人群进行分析。
从 2011 年 2 月到2013 年 1 月,447 例患者被随机分配到高 PEEP 组,453 例被随机分配到低 PEEP 组。有 6 例患者被排除在分析之外,其中 4 例是因其撤销同意书,另2 例是因其违反了纳入标准。

研究结果显示,呼气末正压通气的压力中位数分别为:高PEEP组12cm H2O,低 PEEP 组 2 cm H2O。 术后肺部并发症的人数为:高 PEEP 组的 445 例患者中有 174 例 (40%),相比之下,低 PEEP 组的 449 例患者中有 172 例 (39%)。与低 PEEP 组的患者相比,高 PEEP 组的患者出现了术中低血压,并且需要更大用量的血管活性药物。
上述研究结果表明,开腹手术期间采用高呼气末正压通气结合肺复张之法并不能防止术后肺并发症。术中保护性通气策略应该包括低换气量,低呼气末正压通气,且不宜采用肺复张之法。
原始出处
PROVE Network Investigators for the Clinical Trial Network of the European Society of Anaesthesiology, Hemmes SN, Gama de Abreu M, Pelosi P, Schultz MJ.High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial.Lancet. 2014 Aug 9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








值得收藏,学习,谢谢分享
102
#并发#
30
#PE#
32
#Lancet#
26
#PEEP#
37
#肺复张#
38