Hum Reprod Update:生殖障碍的女性拥有更高的不良妊娠结局
2015-12-24 MedSci MedSci原创
背景:生殖障碍和不孕与产科的并发症有相关性,而且对妊娠的结局有负面影响。受影响的患者常常需要借助辅助生殖技术(ART)受孕,高龄产妇的年龄也是进一步的混杂因素。目前的挑战则是剖析因果关系,即决定不孕不育和生殖疾病如何单独或共同影响女性不良妊娠结局,研究其中的相关和混杂因素。方法:检索PubMed上已发表的截止2015年6月的文章,总结所有关于不孕、有生殖障碍的女性的围产儿结局和影响不良妊娠结局的潜
背景:生殖障碍和不孕与产科的并发症有相关性,而且对妊娠的结局有负面影响。受影响的患者常常需要借助辅助生殖技术(ART)受孕,高龄产妇的年龄也是进一步的混杂因素。目前的挑战则是剖析因果关系,即决定不孕不育和生殖疾病如何单独或共同影响女性不良妊娠结局,研究其中的相关和混杂因素。
方法:检索PubMed上已发表的截止2015年6月的文章,总结所有关于不孕、有生殖障碍的女性的围产儿结局和影响不良妊娠结局的潜在机制的证据。
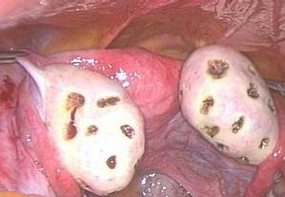
结果:生殖障碍(子宫内膜异位症、多囊卵巢综合征)和不明原因的不孕症共享炎症通路、内分泌异常、蜕膜的衰老和血管异常,这也许会通过共同的机制影响妊娠的成功率。无论是单独还是联合,这些障碍导致早产的风险增加、胎儿成长受限、胎盘疾病和高血压。全身性激素异常、炎症和影响子宫内膜、子宫肌层、宫颈和胎盘的代谢因素与着床和妊娠期间的异常环境有相关性,由此引发产科并发症的发生。这些特征中的一部分已经记录在ART的胎盘部分中。
结论:生殖障碍通常发生在女性的育龄期间,很少是独立存在的。这些障碍具有的相关性炎症、内分泌和代谢机制使产科并发症的发生率增加。这些患者应该意识到不良妊娠结局的高风险,并且应以专业的跟踪检测后续情况。日后需要基于有关临床管理和专业产科护理路径的指南发展,以做出及时的预防性治疗措施。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Update#
36
很有道理!
136
能不能把pmic
127
很值得好学习
171
很有道理
100
#妊娠结局#
26
#不良妊娠结局#
36
#PRO#
30