Nature:肺癌患者的新希望:肺癌研究出现里程碑事件!
2018-01-25 佚名 medicalxpress
肺癌在早期阶段很难发现,而且很难治疗,是全世界癌症死亡的主要原因,估计每年有160万人死于肺癌。然而,新的治疗方法正在改善非小细胞肺癌(NSCLC)患者的患病几率,后者占肺癌患者的85%。。
耶鲁大学医学院医学肿瘤中心主任,耶鲁大学医学与药理学教授Roy Herbst博士说:“在过去的20年中,这方面的进步是巨大的。
传统上,NSCLC已经通过手术治疗,然后通过化疗或放疗或两者都有。 《自然》杂志上发表的一篇综述NSCLC治疗进展的论文的共同主要作者Herbst说:“近年来随着两类药物,分子靶向治疗和最近的免疫治疗的出现,治疗的选择有所改善。(共同作者包括:华盛顿大学医学肿瘤学副教授Daniel Morgensztern博士和辉瑞公司肿瘤学全球产品开发高级副总裁兼耶鲁医学院兼职教授Chris Boshoff。)
分子靶向药物的目的是攻击具有突变基因的肿瘤细胞,例如EGFR,可以导致癌症。美国食品和药物管理局(FDA)于2004年首次批准了用于NSCLC的EGFR抑制剂,目前约有四分之一的NSCLC患者可以接受各种靶向药物的治疗。耶鲁和许多其他机构正在进行研究,以发现更多的分子靶点。但是,患者最终会对这些药物产生耐药性。
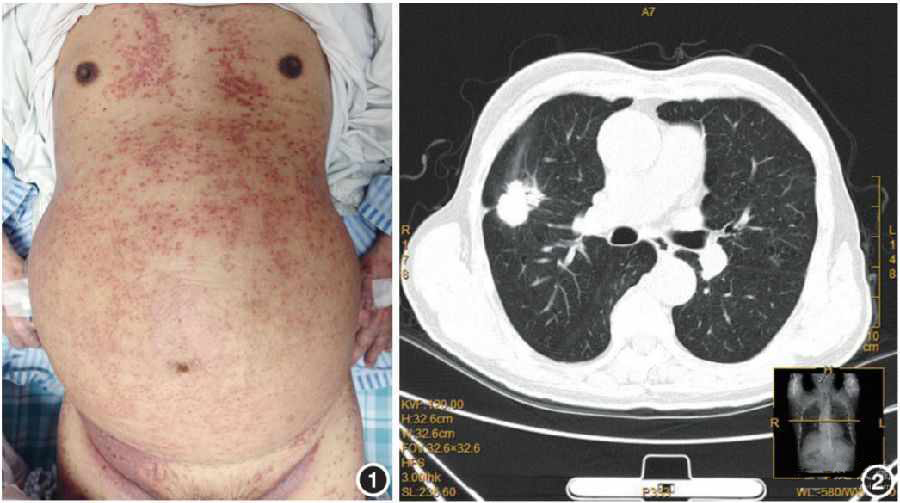
2015年,美国食品及药物管理局批准了第一个“免疫检查点阻滞剂”,为晚期NSCLC患者提供治疗方案。这些免疫疗法阻塞了阻止机体免疫T细胞攻击肿瘤的机制,通过抑制T细胞表面的PD-1蛋白或其在肿瘤细胞上的合作伙伴蛋白PD-L1。肿瘤显示PD-L1水平较高的患者通常是受益于这种免疫疗法的最佳人选。
到目前为止,免疫检查点阻滞剂对大约五分之一的NSCLC患者有效。 Herbst说:“但是,我们已经看到,尽管许多肿瘤表达PD-L1,但许多肿瘤不表达,而PD-L1抑制对这些表达不起作用。即使在PD-L1高表达的肿瘤中,许多在肿瘤微环境中也没有任何T细胞,所以也不管用,我们需要弄清楚我们如何’预热’肿瘤,使他们对这些不同的疗法更敏感。”此外,与靶向治疗一样,大多数肿瘤随着时间的推移对免疫疗法产生耐药性。
Herbst建议,针对免疫系统其他部分的新型免疫疗法将是克服这些挑战的关键。另一个关键是将免疫疗法与化疗、靶向治疗、抑制血管生长的药物或其他形式的癌症治疗结合起来。
Herbst强调说:“我们需要将我们用于靶向治疗的个性化方法转移到免疫治疗,使正确的患者在正确的时间与正确的药物相匹配。
其他研究工作正在创造新的方法来检测肺癌,并追踪每个病人的发展。去年,FDA批准了对NSCLC进行的“液体活检”检测,通过对在血液中循环的肿瘤DNA片段进行测序,可以发现某些类型的EGFR突变。正在开发更高级的“循环游离肿瘤DNA”测试来支持个体化的肺癌治疗。 Herbst说:“液体活检可以让你实时看到事情,而且可以做多次活检,因为它们对病人的侵入性较小。液体活检并不像肿瘤活检那么敏感,但是一些证据表明,他们实际上可以在整个身体上更真实地看待这种疾病。”
NSCLC的临床研究正在加速进行创新的大型临床研究,例如Lung-MAP试验(Lung-MAP),该试验招募了1400多名患者,以测试以前接受治疗的鳞状细胞癌患者。 Lung-MAP正在扩大其范围,以测试靶向药物和免疫疗法的组合。
Herbst指导耶鲁大学的肺癌专业化研究计划(SPORE),肺癌是由国家癌症研究所资助的三个肺癌研究机构之一。该机构汇集了肿瘤学,免疫生物学,药理学,分子生物学,病理学,流行病学和成瘾科学的专家来攻击这一疾病。他说:“我们的目标是把实验室的结果带回诊所,然后再回来。”
Herbst总结说:“总的来说,我们看到了非小细胞肺癌患者前所未有的益处,但这是一个非常艰难的疾病。我们仍然只有30%或35%的帮助。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
25
#新希望#
30
#里程碑#
36
#肺癌患者#
24
好好好好学习学习学习
54
肺癌在早期阶段很难发现.而且很难治疗.是全世界癌症死亡的主要原因.估计每年有160万人死于肺癌.然而.新的治疗方法正在改善非小细胞肺癌(NSCLC)患者的患病几率.后者占肺癌患者的85%..
40
不错啊文章.值得拥有
0
谢谢分享学习了
55
学习了.涨知识
42