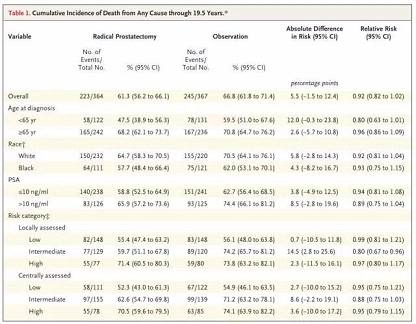
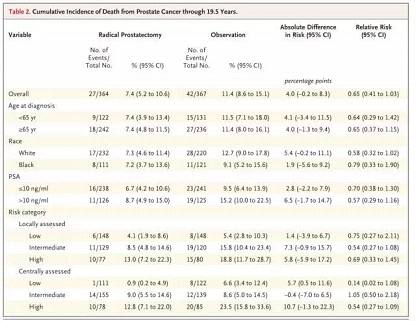
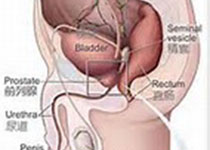
NEJM:长达20年随访发现,与观察治疗相比,前列腺切除术对早期患者无明显益处
2017-07-26 朱爽爽 奇点网
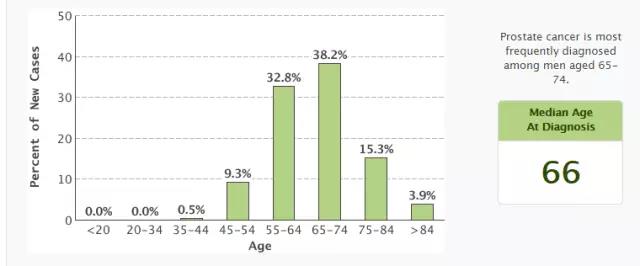
对于每一个被诊断为早期前列腺癌的患者而言,一般会有三个治疗方法可供他们选择:手术、放疗和观察治疗。据2000年的统计数据,只有5.5%的患者会选择观察治疗


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#前列腺切除#
33
#切除术#
38
学习了受益匪浅
68
二十年研究,太难了
77
学习了
83
学习了,谢谢分享
61
谢谢分享,学习了!
0