Cancer Cell:曹雪涛课题组发现肝癌发生和干扰素疗效预判新靶标
2014-01-17 生物谷 生物谷
2014年1月15日,国际肿瘤学研究顶尖杂志《癌细胞》(Cancer Cell,影响因子25分)以封面论文的形式发表了中国医学科学院院长、医学免疫学国家重点实验室主任曹雪涛院士课题组侯晋副教授、周烨和郑媛媛博士及其合作者的研究论文,报道了其发现维甲酸诱导基因-I(RIG-I)在肝癌预后判断、干扰素治疗疗效预判和肝癌发生尤其是男性高发中的作用和机制。该肝癌转化医学研究工作为肝癌预后判断和干扰素治疗疗
2014年1月15日,国际肿瘤学研究顶尖杂志《癌细胞》(Cancer Cell,影响因子25分)以封面论文的形式发表了中国医学科学院院长、医学免疫学国家重点实验室主任曹雪涛院士课题组侯晋副教授、周烨和郑媛媛博士及其合作者的研究论文,报道了其发现维甲酸诱导基因-I(RIG-I)在肝癌预后判断、干扰素治疗疗效预判和肝癌发生尤其是男性高发中的作用和机制。该肝癌转化医学研究工作为肝癌预后判断和干扰素治疗疗效预判提出了新的有效的分子标志物,并发现了RIG-I基因在调控肝癌发生尤其是男性高发中的新机制。【原文下载】
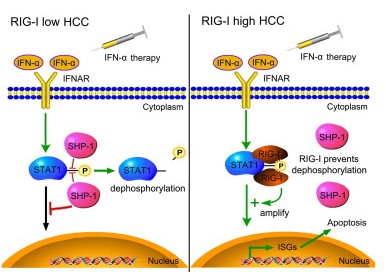
肝癌尤其是乙肝相关肝癌是我国目前的重大疾病,严重危害我国人民健康,干扰素治疗是临床治疗肝癌的重要手段,但部分患者对于干扰素治疗敏感性较差,目前尚缺乏干扰素疗效预判行之有效的分子标志物,使得干扰素临床治疗肝癌面临重大瓶颈。在曹雪涛院士指导下,课题组侯晋副教授、周烨和郑媛媛博士通过与中国医学科学院、复旦大学中山医院、东方肝胆外科医院、香港大学肝病研究所、上海长征医院、中山大学生命科学学院、广西医科大学肿瘤医院、上海交通大学医学院、上海仁济医院、浙江大学医学院第二附属医院等多家单位联合攻关,发现维甲酸诱导基因RIG-I在肝癌中发生了显著的表达降低,并与肝癌患者较差的预后密切相关,因而提出了肝癌预后判断的新靶点。同时,干扰素治疗对于肝癌组织中RIG-I表达较高者有较好疗效,而表达较低者干扰素治疗无效,据此提出了有效的肝癌干扰素治疗疗效预判的分子标志物。分子机制研究发现,RIG-I能够抑制磷酸酶SHP1对干扰素下游效应JAK-STAT信号中STAT1磷酸化活化的负向调控作用,因而增强了干扰素的下游效应信号以维持干扰素长期疗效。此外,课题组还进一步研究了RIG-I在肝癌发生尤其是男性高发中的作用和机制,发现RIG-I在男性肝脏中表达较女性低,而RIG-I缺陷小鼠在肝癌诱导模型中肝癌发生和进展显著加剧,因此提出了RIG-I在肝癌发生中发挥了重要的抑癌基因作用,而男性肝脏RIG-I表达较低可能是肝癌高发于男性的新机制。由此,课题组的该项肝癌转化医学研究提出了RIG-I是肝癌预后判断和干扰素治疗疗效预判的有效分子标志物,并发现了RIG-I在肝癌发生和男性高发中的新机制。
本研究工作是该课题组继2011年发现microRNA-199是肝癌预后判断和基因治疗新靶点(Cancer Cell. 2011; 19: 232-43)之后第二次在肝癌转化医学研究领域取得的重大突破。microRNA-199研究工作曾与"天宫一号和神州八号成功交汇对接"、"蛟龙号载人潜水突破5000米"和"杂交水稻亩产突破900公斤"等成果共同被评选为"2011年中国十大科技进展"。本次工作同样面向我国重大疾病防治需求和医学界目前普遍重视的转化医学研究,在国家"十二五"重大专项、"973"项目和国家自然科学基金资助下,集基础研究、生物技术和临床实验研究等多家单位和学科交叉合作的成果,为肝癌患者的临床治疗尤其是干扰素治疗带来了新的希望。
原始出处:
Hou J1, Zhou Y2, Zheng Y2, Fan J3, Zhou W4, Ng IO5, Sun H3, Qin L3, Qiu S3, Lee JM5, Lo CM5, Man K5, Yang Y4, Yang Y4, Yang Y6, Zhang Q1, Zhu X2, Li N2, Wang Z7, Ding G7, Zhuang SM8, Zheng L8, Luo X9, Xie Y9, Liang A9, Wang Z10, Zhang M11, Xia Q11, Liang T12, Yu Y2, Cao X13.Hepatic RIG-I Predicts Survival and Interferon-α Therapeutic Response in Hepatocellular Carcinoma.Cancer Cell. 2013 Dec 18. pii: S1535-6108(13)00496-0. doi: 10.1016/j.ccr.2013.11.011. 【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#cancer cell#
38
#Cell#
34
#CEL#
43
#曹雪涛#
38
#靶标#
32