Blood:IL10RA调控NPM1-ALK+间变性大细胞淋巴瘤对克唑替尼的敏感性
2020-07-01 MedSci原创 MedSci原创
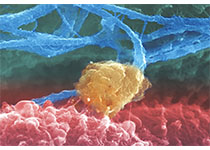
在自分泌循环中,IL10受体绕过NPM1-ALK激活STAT3,以与IL10、IL10RA和IL10RB的启动子结合。
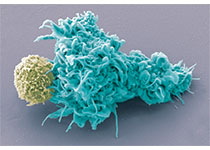
间变性大细胞淋巴瘤(anaplastic large cell lymphoma,ALCL)亦称 ki-1淋巴瘤,是一种T细胞恶性肿瘤,主要由过度激活的间变性淋巴瘤激酶(ALK)融合蛋白驱动。ALK抑制剂(例如克唑替尼)可替代标准化学疗法,其毒性和副作用均较化疗的低。
在临床试验中,由NPM1-ALK融合蛋白驱动的淋巴瘤患儿对ALK抑制疗法的客观缓解率为54-90%。但是,一部分患者在治疗的前3个月内进展。
迄今为止,ALK抑制剂耐药性进展的机制尚不清楚。
通过对ALCL细胞系进行全基因组CRISPR激活和敲除筛选,联合ALK抑制剂治疗后的复发患者的肿瘤细胞的RNA-seq数据,Prokoph等人发现IL10RA异常上调可驱动ALCL对克唑替尼抑制ALK的耐药性。IL10RA表达上调使STAT3信号转导通路重新布线,从而绕过了NPM1-ALK引起的其他关键磷酸化。
IL10RA的表达与ALCL患儿对标准化疗的反应不相关,提示克唑替尼联合化疗可预防ALK抑制剂耐药的特异性复发。
原始出处:
Nina Prokoph, et al. IL10RA Modulates Crizotinib Sensitivity in NPM1-ALK-positive Anaplastic Large Cell Lymphoma. Blood. June 23, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PM1#
25
#ALK+#
38
#细胞淋巴瘤#
27
#敏感性#
28
#变性#
22
#NPM1#
43