JAMA Neurol:芬戈莫德能够减轻颅内出血患者神经功能缺损及促进神经功能恢复
2014-07-23 米怀 丁香园
颅内出血(ICH)后明显的炎症反应会导致血肿周围水肿(PHE)形成、进展并引起继发性脑损害;因此调节ICH患者脑部炎症应该能够减轻水肿,改善临床预后。而芬戈莫德(FTY720,一种鞘氨醇-1-磷酸受体(S1PR)调节器)能够抑制淋巴细胞从淋巴结外出并阻止他们再循环,于2010年被FDA通过用于治疗多发性硬化(MS)。 为了观察芬戈莫德对治疗ICH患者是否安全及能否减轻PHE和神经功能缺损,来
颅内出血(ICH)后明显的炎症反应会导致血肿周围水肿(PHE)形成、进展并引起继发性脑损害;因此调节ICH患者脑部炎症应该能够减轻水肿,改善临床预后。而芬戈莫德(FTY720,一种鞘氨醇-1-磷酸受体(S1PR)调节器)能够抑制淋巴细胞从淋巴结外出并阻止他们再循环,于2010年被FDA通过用于治疗多发性硬化(MS)。
为了观察芬戈莫德对治疗ICH患者是否安全及能否减轻PHE和神经功能缺损,来自我国天津医科大学总医院的施福东教授领衔的团队在新一期的JAMA杂志上发表文章表明:芬戈莫德能够减轻颅内出血患者神经功能缺损及促进神经功能恢复。
此项研究在天津医科大学总医院进行,共纳入了23例血肿体积为5-30毫升的新发幕上ICH患者;临床和神经影像特征匹配病人分为给予口服芬戈莫德组和不给药组。不给药组仅仅给予标准治疗,芬戈莫德组为在标准治疗的基础上加用芬戈莫德;芬戈莫德的给药方案为:在基线CT扫描证实1小时后,症状出现72小时内,口服0.5毫克,连用3天。
主要测量指标和结果为临床评估神经功能状态,MRI监测血肿体积、血肿周围水肿体积(PHE)和相对PHE(定义为血肿周围水肿体积除以血肿体积),共测量3个月。
结果表明,神经功能状态方面芬戈莫德组较不给药组表现出减少的神经功能损害;具体为Glasgow昏迷评分7天时恢复到15分为100% vs 50%(p=0.01),NIHSS评分下降了7.5 vs 0.5(p<0.001);值得注意的是在第一周内改善的神经功能和降低的外周淋巴细胞计数相对应。
在3个月时,芬戈莫德组有更大比例的病人神经功能完全恢复(改良Barthel指数评分95-100分为63% vs 0%,p=0.001;改良Rankin评分0-1分为63% vs 0%,p=0.001;)且拥有更少的ICH相关肺炎。
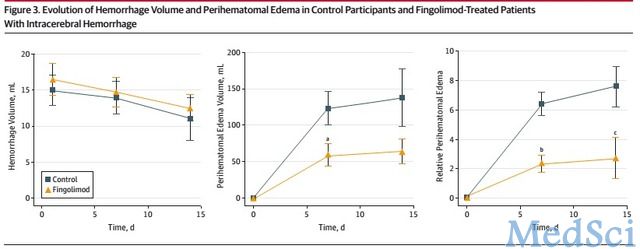
在MRI监测方面,芬戈莫德组较不给药组PHE体积和相对PHE体积明显更小(7天时PHE体积为47毫升 vs 108毫升,p=0.04,;14天时为55毫升 vs 124 毫升,p=0.07。相对PHE体积7天时为2.5 vs 6.4,p<0.001;14天时为2.6 vs 7.7,p=0.003)。不良事件二组之间并没有区别。具体如下图。
关于芬戈莫德的给药方案,作者指出,连续3天的给药能够使淋巴细胞减少持续7-9天,而这也和水肿达到峰值的时间相一致,能够更好地起到作用;又由于任何形式的脑损害包括脑缺血性卒中,能够诱导一个免疫抑制状态,可能超过3天仍旧注射芬戈莫德不但不能提供额外的获益作用,而且延长了免疫抑制状态;并且中和了恢复阶段炎症细胞的组织修复机制。
关于芬戈莫德治疗的机制,其实早在2009年就有用芬戈莫德治疗出血性脑炎的个案报道,而在2011年则在小鼠颅内出血模型中证实了芬戈莫德的神经保护作用及能够提高神经功能结果。在2013年则有动物实验表明芬戈莫德在减少外周淋巴细胞的同时能够减轻脑内淋巴细胞浸润;而且同年动物实验表明芬戈莫德能够减少缺血性卒中tPA后出血转化的发生。
芬戈莫德之所以能在临床试验中得出阳性结果,其机制肯定是多方面的,除了芬戈莫德能够阻止淋巴细胞从外周淋巴结等处浸润到脑这一机制外,芬戈莫德可能对中枢神经系统起到直接的保护作用,因为S1PR在中枢神经系统大部分细胞表达,而芬戈莫德作为S1PR的调节剂,能够随后影响星形胶质细胞、少突胶质细胞和神经元。
而且越来越多的证据表明S1P信号在胚胎中枢神经系统发育和生长,细胞骨架重组,细胞保护,神经干细胞增殖、迁移到神经损伤处起到很重要的作用。
最近则指出了另一个机制即芬戈莫德能够保护血脑屏障的完整性。由于以上三个机制,可能接下来芬戈莫德会应用于更多的脑血管病临床试验,可能较有希望的就是研究芬戈莫德能否延长tPA治疗时间窗、减少tPA后出血转化;而此点动物实验也已证明。
总之这篇文章表明:芬戈莫德能够减轻颅内出血患者神经功能缺损及促进神经功能功能恢复。当然此项试验也存在一些限制,如开放式的设计、样本量小、性别不匹配等。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#神经功能缺损#
45
#Neurol#
38
施教授是做多发性硬化的专家,这次转移到了脑出血领域且发表了如此高分的文章,必有很多东西可以借鉴
145
#神经功能#
38
#功能恢复#
52
#芬戈莫德#
46