Am J Gastroenterol:腹部内脏型肥胖增加肠易激综合征发病风险
2015-01-28 MedSci MedSci原创
腹部脂肪根据区域分布的不同可分为内脏脂肪组织(visceral adipose tissue,VAT)和皮下脂肪组织(subcutaneous adipose tissue,SAT)。已有研究证实,肥胖与一些胃肠疾病有相关性,如糜烂性食管炎、结肠癌、食管癌和胆囊疾病等。但肥胖与肠易激综合征(IBS)的关系还不清楚。 为研究腹部内脏脂肪与IBS发病风险的关系,来自韩国东国大学的Lee CG教授
腹部脂肪根据区域分布的不同可分为内脏脂肪组织(visceral adipose tissue,VAT)和皮下脂肪组织(subcutaneous adipose tissue,SAT)。已有研究证实,肥胖与一些胃肠疾病有相关性,如糜烂性食管炎、结肠癌、食管癌和胆囊疾病等。但肥胖与肠易激综合征(IBS)的关系还不清楚。
为研究腹部内脏脂肪与IBS发病风险的关系,来自韩国东国大学的Lee CG教授等开展一项病例对照研究,成果发表于最近的AJG杂志。
该研究选取2012年1月-2013年8月在健康促进中心曾做腹部CT检查的人群,通过电话随访,根据罗马Ⅲ标准诊断IBS,再将IBS 组与对照组的VAT区域进行对比。通过评估VAT、SAT、VAT/SAT、BMI和腰围来研究腹部内脏肥胖与IBS的关系。同时,Lee教授还研究了内脏肥胖与反流性食管炎的关系。共534人曾做腹部CT检查,研究者排除了8例有下消化道器质性疾病的患者,对526人做了电话随访,最后336人同意参加研究。
共诊断IBS 67例(19.9%),其中腹泻型IBS31例(9.2%),便秘型IBS27例(8.3%),混合型IBS9例(2.7%)。VAT与总脂肪组织(TAT)通过CT测量。(见图1)
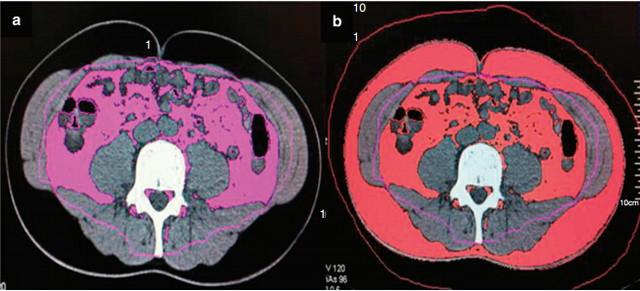
图1、如何测量VAT如图示:(a)VAT;(b)TAT。CT采用容积再现和感兴趣区域相结合。SAT则通过TAT区域减去VAT区域得出。
通过单因素分析得出,IBS组的VAT区域、VAT/SAT、腰围,反流性食管炎发病率以及女性患者比例显著高于对照组。通过多因素分析 得出,VAT区域、VAT/SAT和腰围与IBS发病风险呈独立相关。对于腹泻型IBS,内脏脂肪会增加IBS发病风险。
针对内脏脂肪与IBS呈相关关系的机制,Lee教授提出了自己的看法:1、内脏脂肪位于腹腔内,过多的内脏脂肪堆积可能增加腹腔内压,继 而影响肠道动力。2、内脏脂肪会分泌一系列的脂肪素和细胞因子,可能是引起IBS患者上皮细胞的分泌异常和内脏高敏感性的原因。3、肠道微生物的改变也参 与其中。(见图2)
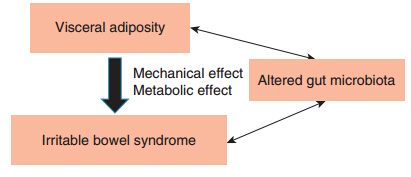
图2、内脏脂肪可能通过机械和代谢两方面作用导致IBS发病。肠道微生物的改变可能同时影响内脏脂肪和IBS。
原始出处:
Lee CG, Lee JK, Kang YS, Shin S, Kim JH, Lim YJ, Koh MS, Lee JH, Kang HW.Visceral Abdominal Obesity Is Associated With an Increased Risk of Irritable Bowel Syndrome.Am J Gastroenterol. 2015 Jan 13. doi: 10.1038/ajg.2014.422.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#GAS#
35
#Gastroenterol#
34
#AST#
31
不错的文章,学习了
101
#综合征#
22