Eur Heart J:不同国家每年经导管主动脉瓣植入的候选人数
2018-04-02 xiangting MedSci原创
每年欧盟和北美地区约有18万名患者可被视为潜在的TAVI候选人。如果TAVI的适应症扩大到低危患者,这个数字可能会升至27万。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











很好
70
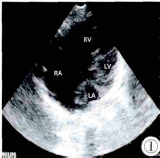
#经导管主动脉瓣植入#
31
高科技主宰人类未来
76
#主动脉瓣#
30
#ART#
22
#主动脉#
26
#经导管#
26
#候选人#
39
#植入#
34
#HEART#
24