COA 2015:张英泽:股骨颈骨折治疗方案选择策略与进展
2015-11-20 MedSci cmacoa
2015-11-19 CMACOA 张英泽 教授 河北医科大学第三医院 中华医学会骨科学分会候任主任委员 股骨颈骨折是临床常见损伤。随着人口老龄化和交通事故的增加,股骨颈骨折的发病率逐年增长。目前,股骨颈骨折已占全身骨折的3.6%,占髋部骨折的48%~54%。由于既往股骨颈骨折后骨折不愈合和股骨头缺血坏死的发生率居高不下,股骨颈骨折一度被称为“尚未解决的骨折”

张英泽 教授
河北医科大学第三医院
中华医学会骨科学分会候任主任委员
股骨颈骨折是临床常见损伤。随着人口老龄化和交通事故的增加,股骨颈骨折的发病率逐年增长。目前,股骨颈骨折已占全身骨折的3.6%,占髋部骨折的48%~54%。由于既往股骨颈骨折后骨折不愈合和股骨头缺血坏死的发生率居高不下,股骨颈骨折一度被称为“尚未解决的骨折”。自1827年法国医生Brulatour报道了股骨颈骨折以来,迄今已经发表近两万篇相关研究报道。随着影像技术及设备、内固定材料及设计、治疗理念及手术技术的进步,股骨颈骨折的治疗效果已得到显著改善,然而,骨折不愈合和股骨头缺血坏死的发生率仍较高。部分创伤骨科医生对股骨颈骨折的认识存在误区,在正确评估骨折严重程度、选择合理规范的治疗方案以及微创复位固定骨折等方面仍然存在不足,影响股骨颈骨折治疗效果的进一步提高。此次应《中国骨伤》杂志社之约撰写有关股骨颈骨折诊断和治疗的述评,笔者认真查阅了国内外相关文献并仔细阅读本期稿件,现简要谈一谈我的观点。
1.正确评估股骨颈骨折损伤严重程度
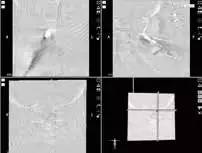
熟悉股骨颈骨折分型有助于正确评估骨折的严重程度。根据最近5年文献报道,较常应用的股骨颈骨折分型有Garden分型、AO/OTA分型、按解剖部位分型、Pauwels分型等,其中以Garden分型应用最为广泛。Garden Ⅰ型是指股骨颈不完全骨折,约占全部股骨颈骨折的2.7%,既往该型骨折常采用非手术治疗,但是保守治疗时骨折往往发生移位,延误诊治,加重患者创伤,而且容易导致骨折断端畸形愈合、延迟愈合,甚至不愈合。Chen等前瞻性分析了825例股骨颈骨折影像资料,利用CT 扫描证实X线片显示的Garden Ⅰ型骨折实际均为完全骨折,应早期对其采取空心螺钉固定,同时应在搬运患者及手术过程中注意避免骨折继发移位。该研究对50年来广泛应用的Garden分型进行了重要修正,提高了骨科医生对Garden Ⅰ型骨折的认识。应用CT扫描有利于对股骨颈骨折细节的观察,可避免二维X线图像因骨折端重叠而错误诊断分型的弊端,不仅有助于早期正确判断骨折损伤严重程度,而且通过三维重建能够直观呈现骨折在各个方向上的移位,有助于选择合理的治疗方案,有针对性地进行复位及固定。基于此,李智勇等制定了股骨颈骨折CT分型方案,根据骨折形态及移位严重程度将其分为无移位完全骨折、横形移位骨折、斜形移位骨折和粉碎性骨折四型,并根据骨折是否存在嵌插或分离移位以及移位的方向,进一步划分为不同的亚型。
2.股骨颈骨折手术方式的选择
对于有多系统合并疾病的高危患者及有手术禁忌证的患者可采用保守治疗,其他患者则建议行手术治疗。常用的手术方式包括闭合复位内固定、半髋或全髋关节置换等。一般认为,对65岁以下的患者可行内固定治疗,对65岁以上的患者可行全髋关节置换或半髋关节置换手术。但是,在临床实践中不能单纯根据患者年龄选择手术方式,笔者设计了成人股骨颈骨折术式选择量化评分表,综合考虑患者年龄、性别、骨折类型、是否存在骨质疏松及其严重程度(骨密度)、生活能力、内科合并症等因素,进行量化评分,根据评分为患者提供规范合理的个体化治疗。
2.1内固定治疗
对于青壮年患者和生理状态很差的高龄患者,可以采用闭合复位空心螺钉内固定治疗。闭合精准复位股骨颈骨折是内固定手术成功的关键,有助于降低术后骨折不愈合和股骨头缺血坏死等并发症的发生率。部分股骨颈骨折不能精准复位固定,其原因有两方面:一是术者经验不足,未能充分掌握复位技巧,术中C形臂X线透视不够,不能详细显示骨折移位方向和程度;二是骨折移位严重,应用常规复位手法难以解剖复位,既往此类骨折常需切开复位固定,创伤大,术后骨折不愈合及股骨头缺血坏死等并发症发生率高。闭合精准复位股骨颈骨折是创伤骨科医生追求的目标,患者麻醉后首先行充分的顺势牵引,通过C形臂X线透视观察骨折移位方向和程度,利用Leadbetter技术、Deyerler技术等手法复位骨折。对于股骨颈嵌插骨折和分离骨折等难复位性骨折,可以通过向股骨头置入2~3枚斯氏针控制股骨头,应用股骨头干三维互动技术实现精准复位。骨折复位满意后植入空心钉导针临时固定,将双下肢置于相同位置,拍摄双侧股骨近端正位X线图像,通过对比患侧和健侧股骨小粗隆的形态(宽度和高度)再次判断骨折复位是否满意,下肢是否存在旋转。在置入导针的过程中,需根据股骨颈干角和前倾角调整导针方向。由于股骨颈前倾角存在性别差异且随年龄增加而改变,因此,建议置入导针时行患侧和健侧透视对比观察,有助于更好地确定导针的置入方向。由于股骨颈移位骨折术后并发症发生率较高,尤其是对伴有其他股骨颈骨折不愈合的高危因素,即年龄大于50岁、女性、高能量伤、美国麻醉协会生理评分(American Society of Anesthesiologists Physical Score,ASAS)Ⅲ级以上,应进行早期干预,可在闭合复位后Ⅰ期植入带双侧皮质的大段髂骨条,采用空心螺钉固定。该技术应用于临床显著降低了股骨颈骨折不愈合发生率。空心螺钉的直径可根据骨折情况来选择。楼宇梁等的研究表明,螺钉直径不会影响股骨颈骨折的愈合时间及术后并发症的发生率。若合并同侧股骨干骨折,可应用股骨重建钉同时固定股骨干和股骨颈骨折。
2.2 髋关节置换治疗
应用髋关节假体置换术治疗股骨颈骨折可以缩短卧床时间,术后早期行功能锻炼,早期恢复患肢功能。有学者认为对于65岁以上的股骨颈骨折患者,只要身体条件允许,皆应进行髋关节置换手术。笔者根据成人股骨颈骨折术式选择量化评分表,对于评分12~17分、身体条件较好、活动能力较强的患者采取全髋关节置换,对于评分18~22分、生理条件较差、活动能力较差的患者选择半髋关节置换。行髋关节置换手术时根据截骨长度选择合适的假体,避免术后双下肢不等长等并发症。笔者应用可调式髋关节置换股骨颈截骨导向器,在术中精确控制股骨颈截骨的角度和高度,根据截骨高度选择合适型号的假体。该技术有效降低了双下肢不等长发生率,提高了手术的治疗效果。
股骨颈骨折的治疗一直是骨科临床工作中的难点,本文从股骨颈骨折的分型、整体评估、治疗方案的选择、手术技术等方面介绍了最新进展,希望为广大骨科医师提供有益的借鉴,以期更加科学合理地制定股骨颈骨折的治疗方案,精确有效地进行手术操作,提高治疗效果,同时降低骨折不愈合和股骨头缺血坏死等并发症的发生率。原载《中国骨伤》
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#治疗方案#
22
#COA#
31
#股骨颈#
29
#股骨#
39
#股骨颈骨折#
44