Blood:突变型钙网蛋白可通过促进TpoR转运,促进癌变的发生
2019-03-23 不详 MedSci原创
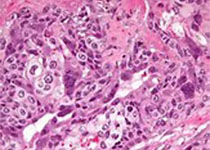
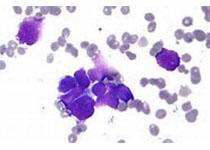
在骨髓及髓外增殖性肿瘤中,钙网蛋白 (CALR) 的第9个外显子上常发生移码突变(+1)。突变型CALRs具有一个新的C端序列,富含带正电荷的氨基酸,可以激活血小板生成素受体(TpoR/MPL)。Christian Pecquet等研究人员发现新序列使突变型CALR获得异常的伴侣蛋白活性,可稳定二聚体状态,并在无法通过质量控制的状态下将TpoR及其突变体运输到细胞表面,这一功能对于致癌转化至关重要
Christian Pecquet等研究人员发现新序列使突变型CALR获得异常的伴侣蛋白活性,可稳定二聚体状态,并在无法通过质量控制的状态下将TpoR及其突变体运输到细胞表面,这一功能对于致癌转化至关重要。突变型CALRs通过部分未成熟的TpoR的分泌途径来控制对TpoR的转运,可保护N117链糖基化不被高尔基体进一步加工。
突变型CALRs可以挽救许多加工的或与疾病相关的TpoRs的转运和功能,如导致先天性血小板减少的TpoR/MPL R102P,也可以克服TpoR上的内质网滞留信号。突变型CALRs除了需要TpoR N链糖基化,还需要TpoR胞外结构域上的疏水斑块诱导TpoR的热稳定性和胞内初始化激活,完全激活则需要TpoR定位在细胞表面。因此,突变型CALRs是TpoR和转运缺陷的TpoR突变体的恶性伴侣,可促进癌症的发生。
Christian Pecquet, et al.Calreticulin mutants as oncogenic rogue chaperones for TpoR and traffic-defective pathogenic TpoR mutants.http://www.bloodjournal.org/content/early/2019/03/22/blood-2018-09-874578
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#突变型#
28
#转运#
0
#TpoR#
31
#钙网蛋白#
28
#癌变#
53