Nature Metabolism:抗癌又抗衰,心脏病药物大放异彩!
2019-10-25 Paris 转化医学网
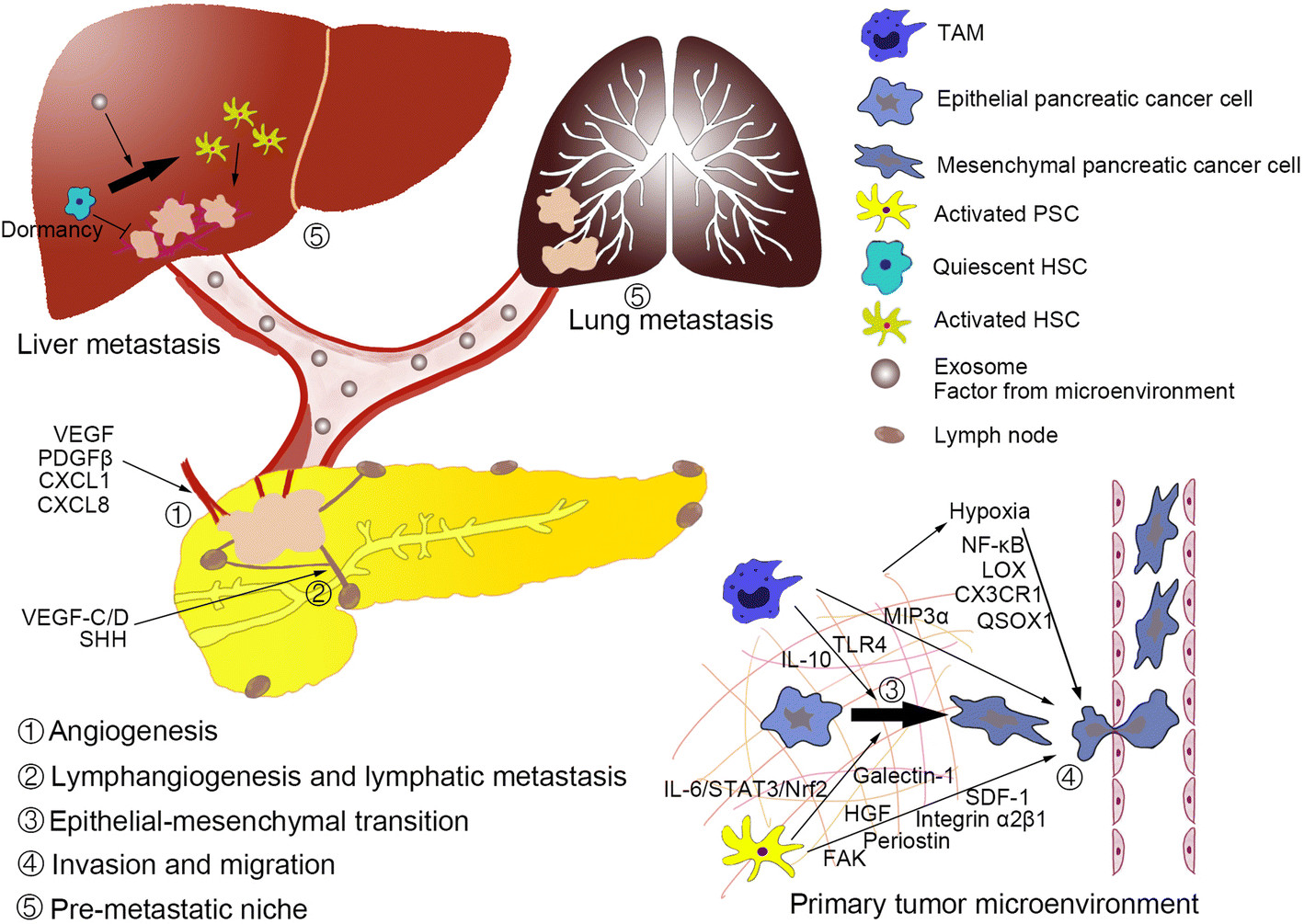
衰老--人类亘古不变的话题,即便在众多疾病侵袭的当今,也依然作为研究热点而存在,在过去的十年中,科学家们发现衰老细胞在越来越多的疾病中发挥着重要作用,从关节炎到动脉粥样硬化,甚至在癌症患者中起到了至关重要的作用。而我们已知的抗衰老药物却总会引起各种各样的毒副反应。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Meta#
28
#MET#
34
#Nat#
30
#Metabolism#
28
#ABO#
30