ANN ONCOL:液体活检RAS可指导mCRC一线抗EGFR治疗
2017-08-10 月下荷花 肿瘤资讯
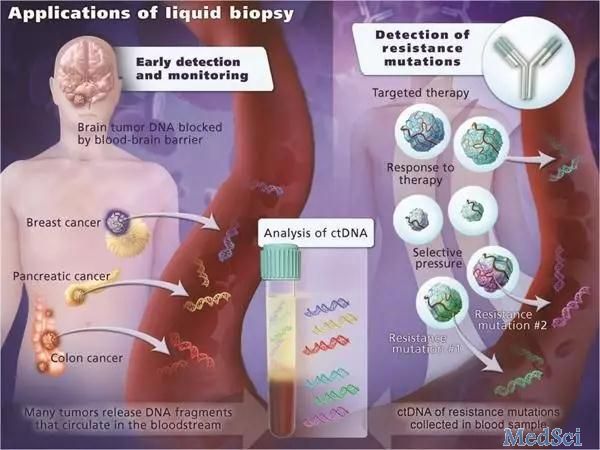
目前没有数据能证实血浆RAS和mCRC结果具有相关性,现有血浆RAS检测仅限于二、三线抗EGFR治疗。意大利的Normanno教授在ANNALS OF ONCOLOGY杂志发文,评估mCRC时液体RAS结果在一线抗EGFR治疗中的价值,结果显示一线抗EGFR单抗治疗mCRC时,液体RAS检测与组织RAS检测的结果相似。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oncol#
28
#mCRC#
27
#CRC#
20
学习啦!谢谢分享!
48
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。给点赞啦
49
文章不错,赞赞赞
43
认真学习,不断进步,把经验分享给同好。点赞了!
49
不错的,学习了!谢谢分享!
48
#活检#
22
#GFR#
19