【一般资料】
患者,女,71岁
【主诉】
右肩疼痛、无力、活动受限1个月,加重1周入院。
【现病史】
患者1个月前无明显诱因出现右肩疼痛,休息及活动时均疼痛,有夜间痛,伴无力、活动受限,抬肩痛,梳头、脱上衣困难,无背手困难。当地医院行MRI检查示右肩关节滑膜软骨瘤或色素绒毛结节性滑膜炎(PVNS),待查。予以静脉注射药物(具体不详)等治疗,症状无明显缓解,近1周来觉疼痛加重,来我院求治。
【体格检查】
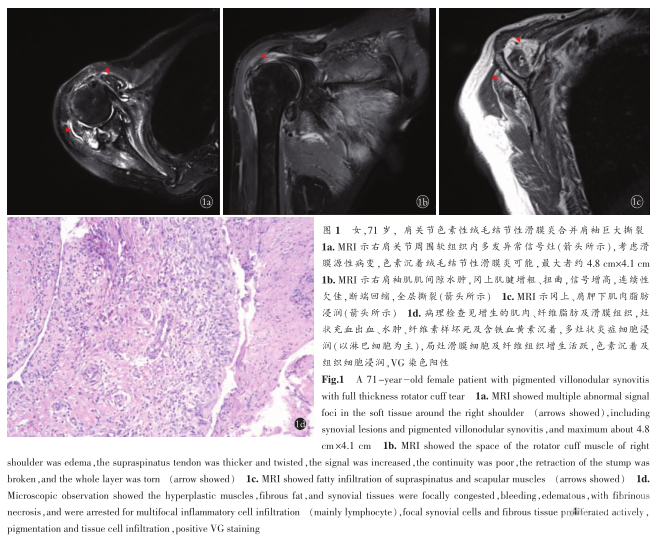
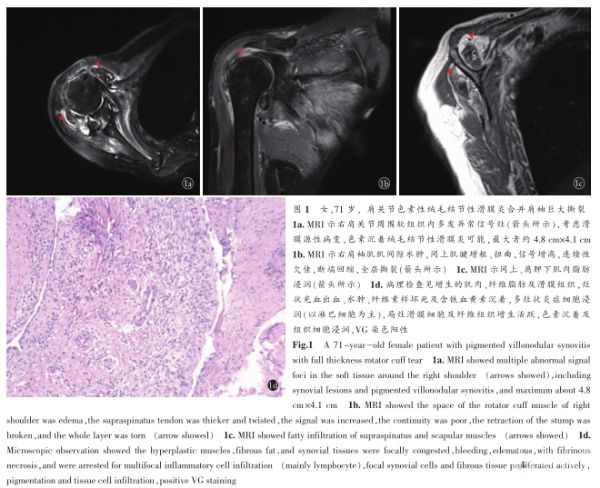
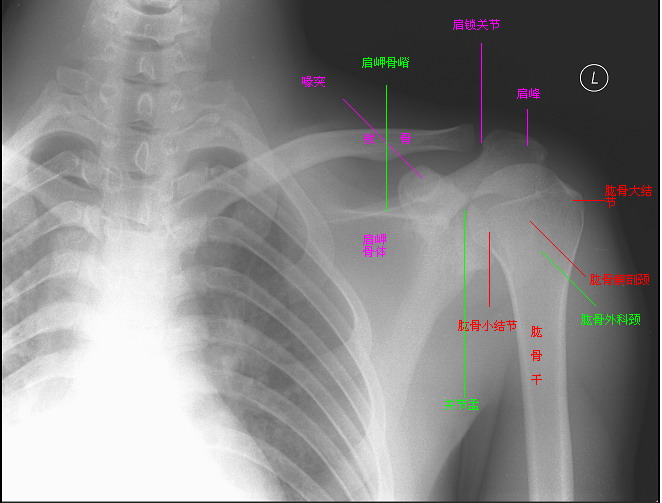
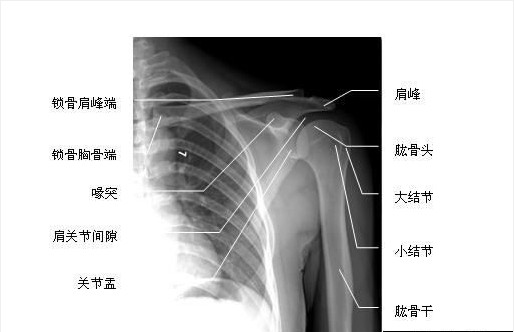
视觉模拟评分法(VAS)评分6分,右肩关节无畸形,无发红,稍肿胀,皮温不高,大结节压痛阳性,Neer征阳性,外展抗阻阳性,前屈抗阻阳性,外旋抗阻阳性,倒罐头试验阳性,拥抱试验阳性,熊抱试验阳性。关节活动度:前屈主动90°,被动110°;外展主动100°,被动120°;后伸主动30°,被动30°;0°外旋主动15°,被动30°;90°外旋主动60°,被动60°;90°内旋主动45°,被动45°。右肩关节MRI见图1a,1b,1c。
【治疗】
患者于全麻插管下行右肩关节镜检、全滑膜切除、肩峰下滑囊清理、肩袖缝合术,探查见肩关节内滑膜大量充血、增生,呈黄褐色,向肩袖间隙及腋囊方生长,下盂唇被病变侵蚀,剥离,予以刨刀清理滑膜、新鲜化处理盂唇。盂肱上韧带、盂肱中韧带、盂肱下韧带均有侵蚀,张力欠佳。肩峰下间隙,可见肩峰下滑囊增生,大量黄褐色病变滑膜沿冈下肌表面和三角肌下表面生长。刨刀及射频清理病变滑膜组织和增生滑囊,冈上肌腱全层撕裂,约100px,撕裂呈反L形,断端回缩至盂上,清理骨床,沿软骨缘植入4枚带线锚钉,垂直褥式缝合肩袖,拉紧打结,侧侧缝合冈下肌和冈上肌之间。术中最大程度保留残留肩袖组织以供缝合修复,彻底清除病变滑膜,由于侵犯范围广泛,嘱术后6~8周行放射治疗。患者术后第1天明显感觉症状好转,VAS评分3分;术后2周切口拆线出院,VAS评分1分,关节活动度较前改善,前屈被动130°,外展被动150°。术后部分滑膜送病理检查可见增生的肌肉、纤维脂肪及滑膜组织,灶状充血出血、水肿、纤维素样坏死及含铁血黄素沉着,多灶状炎症细胞浸润(以淋巴细胞为主),局灶滑膜细胞及纤维组织增生活跃,色素沉着及组织细胞浸润,VG染色阳性(图1d)。
【讨论】
发病机制。色素性绒毛结节性滑膜炎发病原因不明,病因及发病机制至今仍不清楚,有争议的病因主要包括创伤及关节内出血、血脂异常、慢性炎症反应、肿瘤侵蚀等。方斌等研究发现,24例中9例有创伤史提示关节创伤出血可能是PVNS发病原因之一,恰巧本例患者4年前也有过一次肩关节外伤史,故笔者认为外伤是PVNS发生或病情发展一个重要因素。外伤后炎性细胞浸润、关节腔内有渗出液,滑膜细胞、纤维组织及毛细血管大量增生而形成绒毛样结构,当绒毛集结融合成结节时,炎症增生过度到肿瘤性增生,因此该病兼具肿瘤与炎症两种性质。由于肩关节腔空间狭小,滑膜过度增殖,绒毛集结成结节状,形成关节腔内占位性病变,关节腔内压力增高,不断侵蚀邻近组织,如肩袖、软骨等,进而引起肌腱变性,撕裂。分类和发病部位。临床上根据病变部位和范围,可分为弥漫型和局限型两种,位于关节滑膜者多呈弥漫型,位于腱鞘及滑囊多为局限型,多为单发,多发者少见,好发于髋、膝、踝、肘等大关节,另外也有颞下颌关节发现PVNS的文献报道。临床表现及鉴别诊断。初发时常没有明显症状,发现时往往已经侵犯周围组织,故常常被误诊或者漏诊,如发生于足部,误诊为黑色素瘤;发生于踝关节误诊为血管瘤;发生于腹部误诊为腹壁疝;还有误诊为骨巨细胞瘤的报道。诊断失误必然引起治疗方向错误,延误最佳治疗时机。故临床上所有关节内外发现滑膜颜色改变,均应想到有本病可能,最后诊断有赖于术中取病变组织做病理检查。手术中即使肉眼所见滑膜呈黄褐色,有不同程度充血、水肿、增厚,甚至有绒毛或绒毛结节状改变或软骨表面有黄褐色滑膜血管翳覆盖,也不一定就是PVNS,因为上述改变,都可由于出血、含铁血黄素沉着所致,不是本病惟一特征,在滑膜细胞中间必须杂有吞噬含铁血黄素的多核细胞和吞噬类脂质的泡沫细胞才能做出本病的诊断。治疗。对于局限性PVNS,单纯手术滑膜切除可以彻底治愈,将病变滑膜彻底切除,是治疗本病的最有效方法。但对于弥漫性PVNS,要想全部彻底的清除病变滑膜几乎是不可能的,因为关节镜仍然无法到达所有的关节间隙,任何关节滑膜清除术后复发概率都达40%。且本病具有侵袭性及恶变倾向,李平等曾报道膝关节色素绒毛结节性滑膜炎恶变1例,所以术后辅以放疗就显得很有必要。Mollon等报道,对166例弥漫型色素沉着绒毛结节性滑膜炎(DPVNS)患者术后进行辅助放疗,复发率明显降低。因此,放疗是DPVNS安全、有效的辅助治疗方法。不过放疗剂量选择仍存在争议,且由于放疗诱导的器官特异性癌症风险同样不能被忽略。Chida等研究认为,对于膝关节、髋关节弥漫性色素性绒毛结节性滑膜炎患者术后行放疗膀胱癌、结肠癌风险明显增加,故放疗前对患者的评估与告知及放疗后随访注意事项需临床医师谨慎待之。另外,采用中药治疗疗效较好,陈超勇等采用关节镜配合中药桃红四物汤口服治疗膝关节色素性绒毛结节性滑膜炎疗效满意。不过,对于这种合并肩袖损伤老年患者,是不是一定需要同时修复病变肩袖,还有待进一步研究。有文献报道,PVNS合并肩袖巨大撕裂患者,予以关节镜下清除滑膜,肩袖损伤不予处理,术后疼痛症状同样明显改善,不过肌力与关节活动范围并无改善,所以术前与患者及家属沟通,详细告知什么样手术方式能帮助解决哪些问题同样非常重要。总之,关节镜下切除滑膜是治疗肩关节PVNS一种有效手段。目前已经有5家国际临床试验机构着力于研究生物抑制剂靶向治疗,但与局部放射及同位素治疗一样,均未能成为治疗PVNS的金标准,因此一种标准化的治疗策略还有待于进一步明确制定。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#色素#
27
#色素性#
38
#结节性#
30
#肩关节#
33
#滑膜炎#
30
学习了.谢谢分享.
70
谢谢分享学习了
54