J Thorac Oncol:肺癌胸腔积液细胞PD-L1表达是肺癌患者免疫治疗的预后指标吗?
2018-02-27 慧语 肿瘤资讯
恶性胸腔积液是肺癌患者常见的并发症之一,有研究报道在患者的胸腔积液中发现了肿瘤诱导的免疫抑制。根据患者胸腔积液细胞中PD-L1免疫组化染色强度预测免疫治疗反应尚无报道。本研究的主要目的是探索肺癌患者胸腔积液中的肿瘤细胞、免疫细胞及巨噬细胞的PD-L1表达与患者免疫治疗疗效间的关系。
恶性胸腔积液是肺癌患者常见的并发症之一,有研究报道在患者的胸腔积液中发现了肿瘤诱导的免疫抑制。根据患者胸腔积液细胞中PD-L1免疫组化染色强度预测免疫治疗反应尚无报道。本研究的主要目的是探索肺癌患者胸腔积液中的肿瘤细胞、免疫细胞及巨噬细胞的PD-L1表达与患者免疫治疗疗效间的关系。
背景
KEYNOTE-001研究结果发现,PD-L1高表达的NSCLC患者从pembrolizumab中获益最大,特别是PD-L1表达高于50%的患者,客观缓解率(ORR)、中位无进展生存(PFS)、总生存(OS)显着好于低于50%的群体。KEYNOTE 010 和 KEYNOTE 024的研究结果也显示肿瘤细胞PD-L1表达与患者的生存获益有关。但KEYNOTE研究是针对于活检肿瘤样本中PD-L1的表达情况进行评估,本研究针对肺癌伴胸腔积液的患者,期望从胸腔积液中发现对预后敏感的标志物。
方法
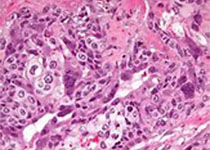
回顾性分析了2014-2016年期间接受了恶性胸腔积液引流的病人,并同时收集了病人的积液细胞块标本。患者治疗后响应根据实体瘤反应评价标准(RECIST1.1)判定,PFS和OS作为生存结局指标评价疗效。为所有细胞块标本的肿瘤细胞、免疫细胞和巨噬细胞的PD-L1采用两种抗体(SP142和22C3)进行了免疫组化染色。细胞免疫活性根据其染色的强度分为四个等级,即:0 无着色、1 弱着色、2 中着色、3 强着色。同时收集了患者的其它临床病例特征数据。
结果
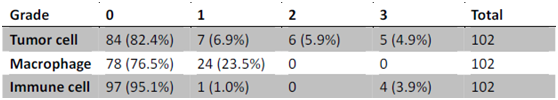
共有102例细胞块适合做PD-L1染色,各类细胞的染色强度结果见表1。胸腔积液肿瘤细胞的PD-L1表达与巨噬细胞和免疫细胞上的PD-L1表达相关(P < 0.01),但巨噬细胞和免疫细胞上的PD-L1表达却不相关。肿瘤细胞的PD-L1表达还与性别(P = 0.012)、吸烟状态(P = 0.032)及ECOG状态(P = 0.017)等人口学特征相关。免疫细胞上的PD-L1表达与患者的总生存率OS相关(P = 0.004)。
表1 各类细胞中PD-L1表达强度结果
此外,回顾研究的患者中有12人接受过免疫治疗,其中5人SD,6人PD,1人失访。12个患者的主要肿瘤组织中均未发现PD-L1表达,在恶性胸腔积液中仅有1例弱表达。免疫治疗响应组的PFS和OS均较长,分别为4 month vs. 1.4 month (P=0.047),10.1 month vs. 3.7 month (P=0.05)。
结论
免疫交互作用或许存在于胸腔积液肿瘤细胞和巨噬细胞间。肺癌伴有恶性胸腔积液的患者中低免疫细胞PD-L1表达往往预后总生存较差。
讨论
如何找到PD-1/PD-L1治疗敏感的患者群体是近来研究的热点。但目前为止关于PD-1/PD-L1表达与肿瘤患者预后之间尚无统一定论。本文作者对102例肺癌伴胸腔积液的患者进行了PD-L1在肿瘤细胞、免疫细胞及巨噬细胞之间表达的关联性研究,以及PD-L1表达与免疫治疗疗效的分析。但本文接受免疫治疗的患者仅有12例,以Brief Report的形式发表,对于部分环节的描写不是非常具体,另外受制于回顾性研究的性质,对于临床实际指导价值有限。但本文提出的研究思路倒是有值得借鉴的地方,那就是除去肿瘤组织本身以外的其它相关组织(液)中的指标能否联合运用分析,以挖掘出PD-1阻断疗法最适合的患者。
原始出处:
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#肺癌胸腔积液细胞#
30
#Oncol#
17
#THORAC#
33
#肺癌患者#
24
#PD-L1表达#
22
#PD-L1#
32
#预后指标#
37