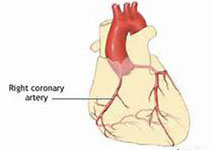
Pharmacotherapy:MI后再灌注 标准治疗β受体阻滞剂受质疑!
2018-06-26 徐钰琦 环球医学
β受体阻滞剂常作为心肌梗死后患者的标准治疗,但支持这一建议的证据主要来自于再灌注前。在再灌注期间,短期(≤30天)β受体阻滞剂治疗被证明可减少心肌梗死(MI)和心绞痛复发,但不能降低死亡率。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#质疑#
28
#阻滞剂#
30
#Pharm#
28
#pharma#
32
#ERA#
33
#标准治疗#
22
#受体阻滞剂#
23
#MAC#
31
#β受体阻滞剂#
33
学习了.长知识
65