Nat Neurosci:卞修武院士等团队在神经胶质瘤取得新突破
2018-12-18 华华中中 iNature
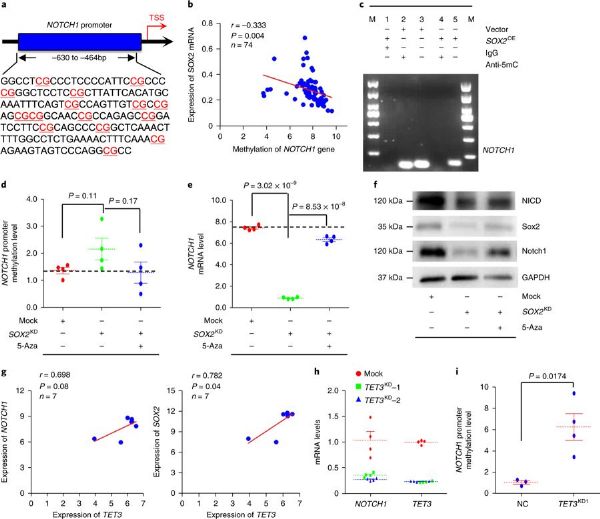
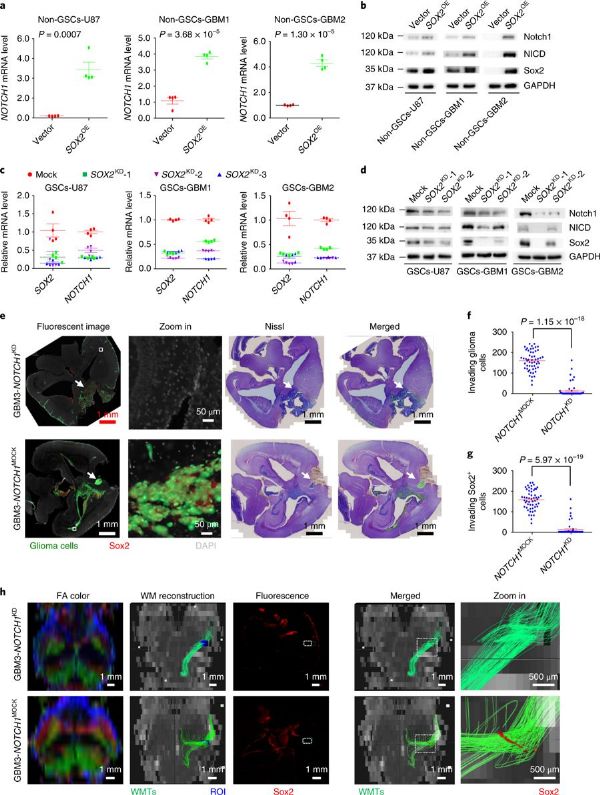
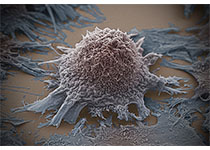
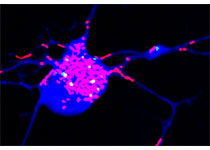
恶性神经胶质瘤是中枢神经系统中最常见的原发性恶性肿瘤。尽管手术,放疗和化疗治疗取得了进展,但这类肿瘤患者的总体5年生存率仍<10%。沿着白质束,血管周围空间和脑膜的早期侵入性生长是恶性胶质瘤最突出的临床病理学特征,并且被认为是治疗结果差的主要原因之一。重要的是要了解胶质瘤细胞是否随机到达这些现有结构,然后为这些细胞的存活提供优势。不幸的是,关于此的知识是有限的。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Nat#
35
#新突破#
40
#神经胶质瘤#
0
#ROS#
35
院士是学术至高点,也是大家必争之地呀
44