手术切除联合光动力治疗骶尾部藏毛窦8 例
2020-01-12 陈娜 杨明霞 张良 中国皮肤性病学杂志
骶尾部藏毛窦是指骶尾部臀间裂处软组织内的 一种慢性窦道,内藏毛发,表现为骶尾部急性脓肿, 反复破溃形成慢性窦道[1]。此病以男性青年发病 为主,白种人多见,黑种人和黄种人发病率较低,且 易于反复发作,治疗困难。2014 年 1 月 - 2018 年 12 月本科收治藏毛窦患者8 例,采取综合性治疗方 式,取得良好效果,结果报告如下。
骶尾部藏毛窦是指骶尾部臀间裂处软组织内的 一种慢性窦道,内藏毛发,表现为骶尾部急性脓肿, 反复破溃形成慢性窦道[1]。此病以男性青年发病 为主,白种人多见,黑种人和黄种人发病率较低,且 易于反复发作,治疗困难。2014 年 1 月 - 2018 年 12 月本科收治藏毛窦患者8 例,采取综合性治疗方 式,取得良好效果,结果报告如下。
1 临床资料
1. 1 一般资料 收集的8 例患者均为2014 年1 月 -2018 年12 月本科收治的明确诊断为“藏毛窦”的 患者,诊断严格按照藏毛窦的诊断标准[1],患者均来自武汉及周边地区,具有完整详细的病情记录。 患者均为男性,年龄 17 ~ 42 岁,平均( 23. 58 ± 6. 27) 岁; 病程 1 ~ 10 年,平均 7. 38 年。8 例患者 中, 3 例初诊为“肉芽肿”, 2 例诊断“肛周脓肿”, 3 例首诊“藏毛窦”。8 例患者均多次于外院进行抗感 染及换药治疗,其中 4 例患者曾进行手术切除及单 纯缝合治疗,均于1 ~2 年后出现复发。临床表现为 骶尾部正中线或偏中线2 cm 以内有1 ~2 个皮下硬 结及窦口,硬结直径约1 ~2 cm,暗红色,表面光滑, 边界尚清楚,浸润部明显,有轻度压痛,表面可见破 溃结痂及窦道。直肠指检及肛门镜检查均未见异常( 图1) 。
1. 2 实验室检查 8 例患者均行经肛管彩超( 以排 除肛瘘) , X 线平片( 排除骨髓炎) 及组织病理检查。 经肛管彩超示:骶尾部包块处局部皮下可见境界不 清低回声区,形态不规则,内部回声不均匀,其内可 见不规则无回声区,无回声区内可见密集细小光点 游移。彩色多普勒血管超声( CDFI) 检测显示:其内及周边可见较丰富血流信号。超声提示: 藏毛窦炎 合并脓肿形成。X 线平片示: 未见骨质破坏。组织 病理检查示: 表皮大致正常,真皮内可见表皮样结 构,周围血管增生,伴混合炎症细胞浸润,可见大量 淋巴细胞、组织细胞、浆细胞、嗜酸性粒细胞、嗜中性 粒细胞,并可见胶原增生,部分病例可见毛干断端 ( 图2) 。病理诊断:藏毛窦。
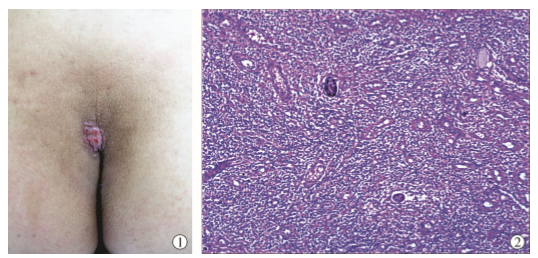
图1 骶尾部偏中线有1 个皮下硬结,直径约2 cm,暗红色,表面光滑,伴绿豆大小窦口,可见破溃结痂,边界尚清楚,浸润部明 显,有轻度压痛; 图 2 表皮大致正常,真皮内可见表皮样结构,周围血管增生,伴混合炎症细胞浸润,可见大量淋巴细 胞、组织细胞、浆细胞、嗜酸性粒细胞、嗜中性粒细胞,并可见胶原增生,部分病例可见毛干断端 ( HE ×20)
图3 使用亚甲蓝经窦口注入,使窦道染色作为术中标示;图4 完整切除窦道、窦道周围、深部所有染色组织,最终深达骶骨 骨膜表面及臀肌筋膜表面
2 治疗及结果
2. 1 治疗方法 手术治疗: 所有患者均行手术治 疗。患者取俯卧位,常规消毒,以利多卡因液局部浸 润麻醉,使用亚甲蓝经窦口注入,使窦道染色作为术 中标示。沿窦口旁开2 cm 作菱形切口,完整切除窦 道及窦道周围和深部所有染色组织,最终深达骶骨 骨膜表面及臀肌筋膜表面( 图 3 ~ 4) 。完整切除所 有受累组织后,仔细凝血,先后以双氧水、碘伏冲洗 创面。光动力治疗: 手术切除即刻,创面以 20% 的 5-盐酸氨基酮戊酸( 上海复旦张江生物医药股份有 限公司) 溶液均匀涂抹,以 8 层纱布覆盖创面,固定 后避光, 4 h 后选择635 nm LED( 型号 FD400-B,武 汉凌云光电科技有限责任公司) 红光进行照射,照 射20 min,能量 120 J/cm2。创面闭合: 术后常规换 药, 1 ~3 d 后待渗出减少,创面肉芽新鲜,行创面闭 合术。8 例患者中4 例以单纯闭合, 4 例以旋转皮瓣 闭合,负压引流管引流,加压包扎。术后常规抗感染 治疗。引流管保留 24 ~ 48 h 后拆除。术后 14 d 拆线。
2. 2 治疗结果 8 例患者伤口均一期愈合,随访 6个月 ~4 年,均无复发。
3 讨论
骶尾部藏毛窦是一种慢性感染性皮肤病,多见 于男性, 17 岁以下者少见, 17 岁以上者逐渐增多, 25 岁达高峰,也有老年人发病的零星报道。藏毛窦发 病机制不详,有可能是局部毛发刺入皮肤而被包裹, 长期刺激导致局部感染和炎症发生[2]。在二战中, 英、美军人的发病率较高,且患者多有长期乘坐吉普 车经历,故又称为“吉普车病”,一般不会发生癌变。 藏毛窦患者多为多毛体质,特别是腰臀大腿部 毛发浓密,本组 8 例患者, 7 例均有多毛体质,仅 1 例腰骶及下肢毛发正常。临床表现为骶尾部的增生 性结节、窦道,反复感染、愈合,再次感染,迁延不愈。 临床诊断时应注意与骶前囊性肿物感染破溃、肛瘘、 肉芽肿、疖、痈及畸胎瘤等疾病相鉴别; 感染的脓肿 可蔓延至肛周或臀部,临床可表现为肛门坠胀,骶尾 部坠、疼痛或反复流脓血,有时引流不畅可伴发热及 白细胞计数升高[3]。体格检查中肛门指诊非常必 要,肛肠内彩超显示肛肠部无瘘管是排除肛瘘的金 标准。组织病理呈慢性肉芽肿性改变,伴有毛干异常堆集或残留,对本病诊断有提示意义,但组织中是 否有毛发并不是诊断的唯一依据。术前的彩超和/ 或螺旋 CT、磁共振成像( MRI) 等辅助检查有助于本 病的诊断及术前确定窦道的范围与深度。 本病治疗首选手术,但单一的手术切除方法,特 别是不彻底的切除将有很高的复发率。手术中需要 充分暴露并清除窦道组织。术前的定位可以有效提 高切除的彻底度。定位包括窦道 MRI 定位、亚甲兰 注射等,术中根据染色范围进行彻底切除。本研究 中的8 例患者按照染色范围切除,创面范围平均达 15 cm ×10 cm,深度均到达骶骨表面及臀大肌深筋膜。 8 例患者术后均采取了即刻光动力治疗。光动 力疗法( photodynamic therapy, PDT) 因其光毒性具 有选择性细胞坏死,免疫调节,抑制清除细菌生物 膜、抗炎及杀菌作用,已广泛用于囊肿性痤疮、头部 穿掘性毛囊周围炎的治疗中。其主要机制仍不甚清 晰,可能是: ①可以调节免疫系统,导致 T 细胞凋 亡; ②PDT 可抑制多种病原微生物的生长,通过抗菌 的作用从而抑制炎症的过程[4]。因红光的穿透深 度为6 mm,创面封闭后再进行光动力治疗药物渗透 性以及照射深度均无法达到要求,以往研究在病变 皮肤上直接进行照射,复发率很高,本研究采取术中 创面旷置敷药进行照射,使 PDT 直接作用于深部炎 症区域,加强抗炎及杀菌作用[5]。 本研究术中即刻采取光动力治疗的原因如下: ①藏毛窦中央坏死组织与周围组织分界不清,即使 有亚甲兰标记,也无法完全定位,从而导致切除不净; ②术中光动力可以直接作用于溃疡表面,减少创面细 菌生长;③光动力治疗对溃疡生长有促进作用[6]。
术后待渗出减少( 一般 2 ~ 3 d) 后行创面闭合 术。闭合创面除了单纯闭合方式以外,经典 Limberg 皮瓣转移、 Karydakis 皮瓣转移术、 V-Y 皮瓣转移术、 Z 型皮瓣转移术、 Bascom 臀沟抬高术等[7]也可采 用。转移皮瓣的目的是为了减少臀中裂处的手术瘢 痕,改变原本较深的臀中裂,从而减少复发。 综上所述,采取术前亚甲兰定位,手术完整切除 病变组织,术中即刻光动力治疗,皮瓣闭合创面的方 法综合治疗骶尾部藏毛窦,具有操作简单、并发症 少、复发率低等优点。
参考文献略。
原始出处:
陈娜,杨明霞,张良,苏飞等,手术切除联合光动力治疗骶尾部藏毛窦8 例 诊疗分析[J],中国皮肤性病学杂志,2019,33(12):1392-1295.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#光动力治疗#
58
#骶尾部#
42
#手术切除#
50
#藏毛窦#
42
#光动力#
31