Antioxid Redox Signal:新发现有望帮助非愈合性创伤患者的组织血管生成
2017-10-12 佚名 “药明康德”微信号
糖尿病的并发症之一是下肢血管病变,引起足部溃疡和坏死,严重者需要截肢。由糖尿病导致的截肢仅仅在英国每天就有20起之多。为了帮助患者提高生活质量,降低社会医疗成本,科学家在进行研究试图改善这个状况。近日,由英国的University of Exeter以及University of Bath的科学家进行的一项研究,报道了脱氧核糖-1-磷酸(deoxyribose-1-phosphate)分子在刺激新
糖尿病的并发症之一是下肢血管病变,引起足部溃疡和坏死,严重者需要截肢。由糖尿病导致的截肢仅仅在英国每天就有20起之多。为了帮助患者提高生活质量,降低社会医疗成本,科学家在进行研究试图改善这个状况。近日,由英国的University of Exeter以及University of Bath的科学家进行的一项研究,报道了脱氧核糖-1-磷酸(deoxyribose-1-phosphate)分子在刺激新血管生成方面的作用,这项发现显示,人体的自我修复系统有潜力帮助治疗糖尿病足这样的非愈合性创伤(non-healing wounds)。该论文发表在《Antioxidants and Redox Signaling》期刊上。
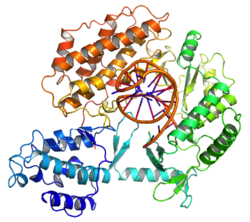
新的血管生成在人体对损伤做出反应时至关重要。该研究表明,脱氧核糖-1-磷酸能激活一种名为NADPH oxidase 2(NOX2)的酶,从而刺激转录因子NFkB,NFkB负责开启特异性参与新血管生成的基因。在血管生成过程中得到激活的一系列基因里,血管内皮生长因子受体2(VEGFR2)起着核心作用。
团队领导者,University of Exeter医学院的Giordano Pula博士说:“我们非常高兴能够发现关于这个关键分子如何刺激新血管生成的新见解,我们现在希望能够在需要组织生成的患者,比如糖尿病足患者中,利用这些知识来触发新生血管的形成。”
Pula博士的团队现在计划着重研究脱氧核糖-1-磷酸通过增加伤口和非愈合性溃疡的血管生成来刺激皮肤修复的能力。该团队希望能开发出治疗诸如糖尿病足这类疾病的新疗法。
原始出处:
Vara, D., et al., Direct Activation of NADPH Oxidase 2 by 2-Deoxyribose-1-Phosphate Triggers Nuclear Factor Kappa B-Dependent Angiogenesis. Antioxid Redox Signal, 2017.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#Signal#
24
#Sign#
37
#新发现#
32
#创伤#
37